Team Member Guide to Benefit Enrollment
Franciscan Missionaries Of Our Lady Health System
My Bene昀椀ts 2023 Team Member Guide to Bene昀椀t Enrollment
Information Resources Your 2023 Total Rewards Just as our team members are more than job descriptions and titles, our rewards program is more than just compensation and bene昀椀ts. Total Rewards is our commitment to provide value to you and your family throughout your career at Franciscan Missionaries of Our Lady Health System. It combines six distinct areas that you can use to meet your individual and family needs: My Purpose, My Compensation, My Bene昀椀ts, My Personal Growth & Development, My Recognition, and My Health & Well-Being. When all of these components are tied together, they create a Total Rewards package that is unique to our organization. This guide will help you understand more about the rewards available to you as a team member of FMOLHS. Bene昀椀t Education Our goal is to make bene昀椀ts easy to understand so you can make the most of them. We have an interactive online learning experience available on our Total Rewards page. In this interactive learning experience, you can pick and choose the topics you want to dive deeper into. Check out all of the education resources available by visiting the page today. » Click here for the Total Rewards page » Click here for 2023 Interactive Bene昀椀t Education Video or scan the QR code at right to directly access the bene昀椀t education video » Click here to review the FMOLHS EPO and PPO Network » Click here to learn about FMOLHS Network Navigation Resources to help you help 昀椀nd a provider in our network. Have Questions? Need assistance with your Bene昀椀t Enrollment? The FMOLHS askHR Team is available by phone or email. » Phone: 833-482-7547 » Email: [email protected] Note In addition to these resources, we are committed to keeping you informed. Stay up to date on the latest communication and updates through: Oracle Employee Self Service, your FMOLHS email, fmolhs.org/TotalRewards and TeamTalk. 2
Your 2023 Enrollment Options Your enrollment options will be displayed in Oracle Employee Self-Service in the following order: NEW ENROLLEE FUTURE ENROLLEE BENEFIT PLAN FMOLHS HEALTH PLAN HEALTH SAVINGS ACCOUNT (HSA) MEDICAL FLEXIBLE SPENDING ACCOUNT (FSA) Team members who are within their 1st 30 Enroll through Oracle Employee Self-Service calendar days of eligibility may enroll through LIMITED MEDICAL FLEXIBLE SPENDING ACCOUNT (LUFSA) annually during the Open Enrollment period. FMOLHS DENTAL PLAN Oracle Employee Self-Service. VISION PLAN LINCOLN VOLUNTARY EMPLOYEE LIFE Team members who are within their 1st 30 For those outside of their 1st 30 calendar days of LINCOLN VOLUNTARY SPOUSE LIFE calendar days of eligibility may enroll through eligibility, enrollment in coverage is not available. LINCOLN VOLUNTARY DEPENDENT LIFE Oracle Employee Self-Service. Team members who previously waived Team members who are within their 1st 30 coverage must complete evidence of insurability LONG TERM DISABILITY calendar days of eligibility may enroll through online during the Open Enrollment period at Oracle Employee Self-Service. MyLincolnPortal.com for eligibility review. LINCOLN VOLUNTARY ACCIDENT Team members who are within their 1st 30 Enroll through Oracle Employee Self-Service calendar days of eligibility may enroll through LINCOLN VOLUNTARY CRITICAL ILLNESS annually during the Open Enrollment period. Oracle Employee Self-Service. COMPANY-PROVIDED GROUP LIFE INSURANCE Company-provided Basic Life Insurance Eligible Team members are automatically coverage. Team members do not need to enroll. enrolled in the Basic Life Insurance. GROUP BASIC LIFE (COMPANY-PAID) Team members do need to designate a Team members do need to designate a bene昀椀ciary in Oracle Employee Self Service. bene昀椀ciary in Oracle Employee Self Service. 403(b) AND 457(b) RETIREMENT ENROLLMENT PROCESS 403(b) AND 457(b) RETIREMENT PLANS Eligible Team members enroll at Eligible Team members enroll at LincolnFinancial.com/FMOLHS LincolnFinancial.com/FMOLHS You can verify your enrollment and print a copy of your elections in Oracle Employee Self Service by clicking on Me/Bene昀椀ts/My Bene昀椀ts. Note Most bene昀椀ts are effective on the 昀椀rst day of the month following 30 days of employment. Long Term Disability bene昀椀ts are effective 昀椀rst of the month following 6 months of employment. (New Hire date: March 5; bene昀椀ts are effective on October 1.) 3
Table of Contents All eligible Team 5 Important Information Members must enroll 7 Enrollment within 30 days of 11 My Health Bene昀椀ts new hire/new 12 Navigating Our Network eligibility date. 25 My Phar macy Bene昀椀ts 28 Pr eauthorization Requirement List 32 My Health and W ell-Being 35 My Dental Bene昀椀ts 37 My Vision Bene昀椀ts 39 My Health Savings Accounts – HSA 41 My Flexible Spending Account – FSA 43 My Life Insurance 44 My Retirement Bene昀椀ts 47 My Disability Insurance 48 My V oluntary Bene昀椀ts 52 My EAP 54 My Discounts 58 Requir ed Notices 66 Important Contacts In this guide we use the term “Company” to refer to FMOLHS. This guide is intended to describe the eligibility requirements, enrollment procedures, and coverage effective dates for the bene昀椀ts program offered by the Company. It is not a legal plan document and does not imply a guarantee of employment or a continuation of bene昀椀ts. This guide is not intended to answer all of your questions, but to provide you with a tool to answer most of your questions. Full details of the plans are contained in the Plan Documents, which are available on your facility intranet and govern each plan’s operation. Whenever an interpretation of a plan bene昀椀t is necessary, the actual plan documents will be used. 4
Important Information Enrollment for the 2023 Plan Year Complete your bene昀椀t enrollment and submit complete dependent veri昀椀cation documentation within 30 calendar days of your new hire/new eligibility date (e.g. for a new hire date of May 1, enrollment and documentation deadline is May 30). If you meet the income guidelines, apply for the health plan premium reduction, Just Premium, within 30 calendar days of your eligibility date (see page 10 for details). Member Cards Team Members who enroll in the following bene昀椀ts will receive member identi昀椀cation cards: » Medical Cards – FMOLHS Health Plan through Blue Cross Blue Shield (BCBS) » Dental Cards – Delta Dental » Vision Cards – UNUM » Medical Flexible Spending Account (FSA)/Health Savings Account (HSA) – Pay昀氀ex Human Resources Contact Reach out using the method that works best for you: » Submit an Oracle Service Request by clicking on Help Desk/HR Service Requests.* » Email [email protected] » Call 833-4UaskHR (833-482-7547) *This is the fastest method for getting an answer to your question. Note If you (and/or your Dependents) have Medicare or will become eligible for Medicare in the next 12 months, a Federal law gives you more choices about your prescription drug coverage. Please see page 58 for more information concerning Medicare Part D coverage. 5
Important Information Be Healthy. Be Happy. Register for My Health Toolkit to help you get started. You will have anywhere, anytime access to your bene昀椀ts information, insurance cards, claims and covered local providers. Download the My Health Toolkit mobile app. It’s free at: www.MyHealthToolkitLA.com/links/FMOLHS. Get Started Today Why wait? It’s easy to sign up. In just a few clicks, you will have everything you need at your 昀椀ngertips. 1. Go to www.MyHealthToolkitLA.com/links/FMOLHS and select Register Now. 2. Enter the number on your membership card and your date of birth. If you don’t have your membership card, you can enter your social security number. 3. Choose a username and password. 4. Enter your email address and choose to go paperless, if you would like. Your Membership Card Your Blue Cross Blue Shield membership card contains important information that helps providers apply your bene昀椀ts correctly. Keep it with you at all times by downloading your digital ID card to keep on your smart phone. It is all about convenience. Your digital ID card has the same information that your plastic card will have. In 2023, your membership card will now include your deductible and out of pocket maximums. You will be able to: » View your card on your smartphone, tablet or computer » Email the card to a spouse, child, doctor’s of昀椀ce or pharmacy » Print the card from a smartphone, tablet or computer and use the print out just like a plastic card Accessing your Digital ID Card To access your digital ID card through the My Health Toolkit app you will need to follow these instructions: » Log in to My Health Toolkit. Note » From your mobile device, select Insurance Card. Sign Up for My Health Toolkit at: » From a computer select Insurance Card and then www.MyHealthToolkitLA.com/links/FMOLHS View Your Card. 6
Enrollment All eligible team members must enroll online through Oracle Employee Self Service. Things to Consider Qualifying Life Events Include: Before you enroll, it is a good opportunity for you to Enrollment changes based upon a qualifying life event assess your bene昀椀t needs. must occur within 30 calendar days of that event.* (For » Does your spouse have bene昀椀ts coverage available Example: If you get married on March 1st, you must enroll no later than March 30th.) through another employer? » Did you get married, divorced or have a baby » Change in your FTE status from part-time to full-time or full-time to part-time that results in a recently? If so, do you need to add any dependent(s) signi昀椀cant increase or decrease in your premiums or add your bene昀椀ciary designation? » Did any of your children reach his or her 26th birthday (medical or dental) » Change in your legal marital status (marriage this year? If so, they are not eligible for bene昀椀ts. and divorce) » Change in the number of your dependents (for Your Eligible Dependents for Core example, through birth or adoption, or if a child is Benefits Enrollment no longer an eligible dependent) Dependents eligible for coverage in the FMOLHS Bene昀椀t » Change in your spouse’s employment status Plans include: » Your legal spouse. (resulting in a loss or gain of coverage) » Your dependent children up to age 26 (includes » Change in your employment resulting in a gain or loss of coverage stepchildren, legally-adopted children or children » Entitlement to Medicare or Medicaid* placed with you for adoption, foster children and *If you become eligible for or lose coverage under Medicaid or a state child health plan, grandchildren for whom you have legal custody). you must enroll or terminate coverage within 60 days. » Your dependent child, regardless of age, provided he or she is incapable of self-support due to a mental or physical disability, is fully dependent on you for support as indicated on your federal tax return, and is approved by your Health Plan to continue coverage past age 26. » Please note that veri昀椀cation of eligibility will be required once dependents are enrolled. See page 8 for dependent veri昀椀cation requirements. Note All eligible Team Members must enroll within 30 calendar days of new hire/new eligibility date. 7
Dependent Verification ACCEPTED/REQUIRED VERIFICATION DOCUMENTS DEPENDENT TYPE NATURAL CHILD* Birth Certi昀椀cate; for newborns, birth letter from hospital STEP CHILD* Birth Certi昀椀cate AND veri昀椀cation of current marriage between Team Member (Requires current spouse & child and natural parent (see spouse veri昀椀cation requirements below) veri昀椀cation documents) ADOPTED CHILD/CHILD PLACED Adoption Certi昀椀cate/placement letter from court or adoption agency for FOR ADOPTION* pending adoptions FOSTER CHILD* Proof of Legal Custody, such as a court order GRANDCHILD* Proof of Legal Custody, such as a court order AND copy of current tax return that (Requires 2 documents) identi昀椀es grandchild as a taxable dependent SPOUSE Marriage Certi昀椀cate; AND current or previous year tax return face sheet OR proof of current joint ownership (such as a joint mortgage, joint rental (Requires 2 documents) agreement, joint bank account, joint auto insurance etc.) *Less than age 26 regardless of marital or student status Dependent veri昀椀cation documents for any newly enrolled or previously unveri昀椀ed dependents must be received within 30 calendar days of new hire/new eligibility date in order to maintain dependent coverage. FMOLHS reserves the right to audit dependent veri昀椀cation documents at any time. Note Upload Dependent Veri昀椀cation Documents in Oracle Employee Self Service under Bene昀椀ts/My Documents. 8
How to Enroll in Oracle Employee Self Service 1. Understand Your Choices! The Team Member Guide to Bene昀椀ts Enrollment is available by clicking on My Bene昀椀ts on our Total Rewards page. 2. Review Your Personal Information 3. Enroll Online from Work or Home https://eqtm.login.us2.oraclecloud.com 4. Log in with Your Username and Password a. Click the Me tab b. Click the Bene昀椀ts tile » Note: Before starting your enrollment, be sure to review My Bene昀椀t Resources Card for your bene昀椀t options and important notices c. Click Start Enrollment button 5. Add Your Dependents and Beneficiary(s) a. Be sure to complete all required 昀椀elds for each dependent and bene昀椀ciary b. Upload dependent veri昀椀cation documents to Oracle Employee Self Service under Bene昀椀ts/My Documents. 6. Review Your Dependent Child’s Eligibility for Coverage a. Core Bene昀椀ts (Health, Dental, Vision) – To age 26 regardless of marital or student status. b. Voluntary Life Bene昀椀ts – Unmarried dependent children to age 21; to age 25 if a full time student. c. Voluntary Accident and Critical Illness Bene昀椀ts – To age 26 regardless of marital status or student status. 7. Save and Print Your Elections! If your bene昀椀t elections are properly completed and saved, you will get a con昀椀rmation message on the screen that states, "Your bene昀椀t elections were saved.." If you do not receive a con昀椀rmation message, your elections were not properly completed. You must complete the election process again within 30 days of your new hire/new eligibility date. Go to My Bene昀椀ts card to view and print a copy of your elections. You must have a copy of your 2023 bene昀椀t elections to report a problem with your enrollment. 9
2023 Premium Reduction Opportunities – EPO and PPO Medical Plans Team members are required to complete an annual application to determine eligibility for “Just Premium”. “Just Premium” aligns with our Mission and expands the offer of medical plan premium reductions to team members who apply and qualify for 昀椀nancial assistance based on total household income. Based upon your total household income (adjusted gross income), the number of dependents you claim on your 2021 Federal Income Tax Return, your FTE status (only available to full-time team members), and your hourly rate, you and your family may be eligible for the Just Premium reduction. DEPENDENTS LISTED ON TAX RETURN MAXIMUM HOUSEHOLD INCOME 0 to 1 $34,373 2 $35,482 3 $41,026 4 or more $46,570 Current Maximum Hourly Rate $32.00 Approved team members will receive higher FMOLHS medical plan subsidies to improve affordability and access to coverage. Team Members may select from the EPO or PPO Plans for themselves and their eligible dependents. Please submit a completed application and tax return within 30 calendar days of your new hire/new eligibility date. To apply for Just Premium: » Select My Bene昀椀ts on our Total Rewards and then click on the Just Premium Application link. » Print and complete the application and attach a copy of the 昀椀rst two pages of your 2021 Federal Individual Income Tax Return. If you are married, 昀椀ling jointly, submit one tax return. If you are married, 昀椀ling single or head of household, you will be required to submit the 昀椀rst two pages of both your tax return and your spouse’s return. » Return application/tax return(s) to [email protected] or fax 225-765-9307 within 30 calendar days of your new hire/new eligibility date. Note Individuals who did not 昀椀le a 2021 Income Tax Return will not be eligible for the 2023 Just Premium. 10
My Health Bene昀椀ts Blue Cross Blue Shield www.MyHealthToolkitLA.com/links/fmolhs • 833-468-3594 Health coverage is one of the most important bene昀椀ts FMOLHS can provide. Health bene昀椀ts provide signi昀椀cant value through support for and protection against potentially large 昀椀nancial expenses, as well as covering preventive care. FMOLHS is committed to keeping team members healthy and productive by offering comprehensive health care plans. The option you choose will be in place for all of 2023, unless you have a qualifying life event. Health bene昀椀ts will be administered by Blue Cross Blue Shield. How Do I Find a Provider? FMOLHS has a customized provider directory for its Plan members. To see the current list of the FMOLHS EPO Network or PPO Tier 1 or Tier 2 Network providers online, visit www.MyHealthToolkitLA.com/links/fmolhs. If you do not have access to the website, please call Blue Cross Blue Shield Customer Service at 833-468-3594 for assistance. 11
Navigating Our Network Navigate Our Provider Network the Easy Way STEP 1 FINDING AN IN-NETWORK PROVIDER We understand the importance Whether it be our EPO network or our PPO Tier 1 or NOTE: Always verify a of 昀椀nding a healthcare provider Tier 2 network, our Network Guides can help you: provider’s network status by who can best meet the needs • Find a provider in network calling Blue Cross Blue Shield at of you and your family. We also (833) 468-3594 or by logging understand how daunting it might • Check if a provider you are already seeing is on to MyHealthToolkitLA. be to scroll through a list of doctors in network prior to enrollment com/links/fmolhs. You will in search of the best 昀椀t. That’s why • Assist with scheduling an appointment with have access to the EPO and PPO we offer team members a resource network-based primary care physicians Tier 1 and Tier 2 networks at this to help navigate our FMOLHS site. If the provider address customized network. • Check availability of a specialty service They are called Network Guides, within our network listed on the directory is not and they are available in most Call (855) 875-6265 to connect with a Network Guide the address where care will locations by phone 24/7 for team today. You will be prompted to select a guide for either be delivered, the provider members in both Louisiana and our Louisiana or Mississippi network. may not be in network. Mississippi. Contact BCBS to con昀椀rm. STEP 2 ACCESSING CARE IN OUR NETWORK We offer a variety of ways to connect and access care with an FMOLHS primary care provider. Your PCP is responsible for providing comprehensive care, for having knowledge of your overall medical history, and in assisting you with navigating certain health risks and your healthcare journey. In-Person Video Visits Virtual Extended Hours Visits Same great Avoid urgent care or ER fees and Meet face to care from your meet virtually with a FMOLHS primary All appointment types face with your own provider care provider in our network after are available to schedule provider for from the hours for free with the EPO plan or through MyChart for all wellness checks comfort of your for $5 with the PPO Plan. or appointments home. Available in Louisiana only. ages. that need full We’re working to expand this care evaluations. opportunity to Mississippi. STEP 3 ACCESSING CARE OUTSIDE OUR NETWORK If you need services that are not available Submit all completed requests in NOTE: The network within our EPO or PPO Tier 1 or Tier 2 writing via fax to (803) 264-0259, exception MUST be network, Network Exceptions are available. by email to FMOLHSEXCEPTION@ [email protected] requested and approved To receive an exception, you must complete BCBSSC.COM or by mail to: before services are the Network Exception form on the Total Blue Cross Blue Shield rendered. If the request Rewards My Bene昀椀ts page and have it signed of South Carolina is made after services by your provider. Signed and completed Attn: Network Waiver, AX-630 are rendered, it will not forms must be submitted to BCBS of South PO Box 100300 be considered unless Carolina before services are rendered to be Columbia, SC 29202 otherwise required by law. considered. BCBS SC will notify you of their decision on your request. 12
Road Map to Care Think of your Primary Care Physician (PCP) as your go-to for your health care needs. Your PCP plays an important role in your healthcare journey. Ultimately, building a relationship with your PCP and going to them regularly for illnesses, yearly checkups and screenings can lead to better health outcomes and a higher level of satisfaction with care. In need of a Primary Care Physician? Our Network Guides can help you 昀椀nd a provider. Call now at 855-875-6265. First Stop Primary Care Physician (PCP) Having one doctor who knows your overall health history and can better guide you as you navigate certain health risks leads to better patient experience. There are several ways you can connect and receive care from your in-network PCP, through in-person visits to convenient virtual visits like video or virtual extended hours. See our network navigator page to learn more about each care opportunity available in your area. Second Stop If it's the weekend or it’s later in the evening, Virtual Extended Hours and Urgent Care are good options to consider. Third Stop There are several medical conditions that are considered emergencies because treatment is only available in a hospital setting. 13
Which Plan Is Right for Me — the EPO Plan, PPO Plan or HDHSA Plan? Choosing the most cost-effective health plan is more than just signing up for the one with the lowest paycheck deduction. EPO Plan The EPO Plan provides access to a narrow network of healthcare providers that are either a part of our health system or considered our preferred partners. This means that the plan will allow for eligible medical services as long as you visit a healthcare provider — doctor, hospital or other place offering health care services — within our narrow EPO network. With this plan, the cost shared by you will be lower, whether that is through premiums, copays, deductibles or your out-of-pocket-maximum limit for the year. The plan offers a $250 individual and $500 family deductible and a $0 copay for PCP of昀椀ce visits. Upon enrolling in the EPO Plan, you will gain access to providers who offer high quality care and who are more clinically integrated with our organization’s electronic medical record system, allowing for more comprehensive care. In addition, you can designate a primary care provider (PCP) that can act as your personal health advocate and coordinate your healthcare. It’s important to know that coverage for medical services outside of the EPO network will only be allowed in the event a medical service is needed that is not available within the network. In an emergency, however, eligible services will be covered. This plan may be a better option for those who would like lower deductibles and copays at time of service as well as overall reduced out-of-pocket expense. PPO Plan The PPO health plan design has higher deductibles, coinsurance and copays than the EPO Plan, and continues to offer out-of-network coverage for most services. The pharmacy design copays remain the same including the specialty copays — $100 if 昀椀lled at RxONE and $150 if 昀椀lled by Express Scripts. If you reside outside of Louisiana or Mississippi, you are eligible for out-of-area coverage at the Tier 2 coverage level if you see a BCBS provider in your home state. The out-of-area coverage is based solely upon the employed team member’s address outside of Louisiana or Mississippi. The PPO has higher monthly premiums, but offers out-of- network coverage if needed. This plan choice is bene昀椀cial for those individuals who need out-of-area coverage or need a broader network coverage including out-of-network coverage. HDHSA Plan The HDHSA Plan design has higher deductibles and out-of-pocket maximums along with FMOLHS funding. FMOLHS will provide $750 individual and $1500 family contribution to your HSA account to help with out-of-pocket medical expenses. The deductibles for the HDHSA Plan are $1,750 individual and $3,500 family. If you can take on more 昀椀nancial risk, perhaps you might consider the HDHSA Plan. With a High Deductible Health Plan and a Health Savings Account (HSA), you can save additional pre-tax dollars to pay for medical expenses. You decide how to spend your dollars. Unused HSA dollars roll over from year-to- year. (There are restrictions and limitations to enrollment in the HSA.) 14
Choosing the health plan that is right for you is important. You want to make sure you’re covered for the year ahead, while ensuring you choose the most effective option based on your personal health needs. CONSIDER CONSIDER CONSIDER THE EPO THE PPO THE HDHSA PLAN PLAN PLAN MY HEALTHCARE NEEDS I HAVE A CHRONIC DISEASE, SEE SPECIALIST PHYSICIANS, AND/ OR TAKE SEVERAL BRAND PRESCRIPTION MEDICATIONS. I AM VERY HEALTHY, HAVE NO PLANNED MEDICAL PROCEDURES, TAKE ONE GENERIC PRESCRIPTION MEDICATION AND ONLY HAVE ROUTINE PREVENTIVE CARE. I HAVE A SURGERY SCHEDULED AND CAN USE TIER 1 PROVIDERS. I AM PREGNANT OR PLAN TO BECOME PREGNANT. I HAVE SAVED DOLLARS TO PAY TOWARD MY DEDUCTIBLE AND CAN AFFORD TO PAY THE CO-INSURANCE COSTS OF MY MEDICAL CARE. I HAVE YOUNG CHILDREN WHO ARE OFTEN SICK OR INJURED. I AM LOOKING FOR A HIGH DEDUCTIBLE PLAN THAT ALLOWS ME TO PAY FOR HEALTHCARE EXPENSES WITH DOLLARS I SAVE ONCE I RETIRE. I SEE A PROVIDER THAT IS IN TIER 3 OF THE PPO NETWORK AND WOULD LIKE TO CONTINUE TO SEE THIS PROVIDER EVEN THOUGH MY OUT OF POCKET EXPENSE IS HIGHER. I WORK REMOTELY IN A STATE OTHER THAN LA OR MS AND NEED TO ACCESS CARE FOR MYSELF AND MY FAMILY How Will I Be Billed for a Physician Office Visit? If you are enrolled in the EPO Plan and choose a provider in the EPO network, your primary care visit will be a $0 copay. There is no coverage outside of the EPO network. If you are enrolled in the PPO Plan, your of昀椀ce visit copay pays for your share of the cost of the of昀椀ce visit. When you have additional services, those services are subject to deductible and coinsurance. All services under the HDHSA Plan are subject to deductible and coinsurance. The chart below gives examples of how services would process under the EPO and PPO Plan. IF YOU HAVE: YOU WILL PAY UNDER EPO PLAN: YOU WILL PAY UNDER PPO PLAN: PCP Of昀椀ce Visit No Cost Copay Specialty Of昀椀ce Visit Copay Copay Injections Included with Applicable Of昀椀ce Visit Copay* Deductible & Coinsurance X-rays Included with Applicable Of昀椀ce Visit Copay* Deductible & Coinsurance Lab work Included with Applicable Of昀椀ce Visit Copay* Deductible & Coinsurance *For some services, coinsurance and deductible may apply. 15
How Will I Be Billed for Medical Services? What If a Medical Service or a Claim Is The chart below gives examples of medical services Denied? What Are My Appeal Rights? that require the attention of a physician who may send a When a claim for bene昀椀ts or service denial occurs separate bill for payment. under the FMOLHS Health Plan, the member receives an explanation of bene昀椀ts (EOB) or service denial letter YOU WILL ALSO RECEIVE IF YOU HAVE: A BILL FROM: explaining the reason for the denial. The member has the right to 昀椀le an appeal to request a review of the denial. X-rays The radiologist The appeal should include policy holder name, health Certain lab tests The pathologist plan ID number, patient name, details regarding the Surgery The anesthesiologist & surgeon claim/service being appealed (such as a claim number), Visit by your personal physician Your personal physician and date and provider of service. For full details, please EKG Cardiologist see the Grievances and Appeals Process in the FMOLHS Health Plan Document posted on your facility intranet. Please note for the PPO Plan: If you have a procedure You must 昀椀le an appeal within 180 days after you have performed at an FMOLHS facility, your provider may or been noti昀椀ed of the denial of bene昀椀ts. may not be a FMOLHS Network Tier 1 provider. If the Send requests for review of a denial of bene昀椀ts by provider is not a FMOLHS Network Tier 1 provider, but mail to: is an in-network provider, you will receive a separate bill Blue Cross Blue Shield from the provider for the services performed and the Columbia Service Center provider will be paid at the Tier 2 bene昀椀t level. Attention: Appeals Coordinator AX-830 For example: if you have elected the PPO Plan (80% P.O. Box 100121 FMOLHS Network Tier 1 / 70% Preferred Provider Network Columbia, SC 29202-3121 Tier 2) you would be responsible for 30% of the in-network anesthesiologist’s bill after you have met your deductible. How Do I View My Medical Claims Online? To register for Blue Cross Blue Shield Online Services, after you receive your new medical ID card visit www.MyHealthToolkitLA.com/links/FMOLHS. You will need your medical ID card to register. » Select Register Now » Select Register » Follow the steps given to register www.MyHealthToolKitLA.com/links/FMOLHS allows you to: » View medical claims » View or print explanations of bene昀椀ts » View, request or print an ID card » Find a network provider 16
Health Plan Summaries The charts below give a summary of the 2023 Health Plans for FMOLHS. All covered services are subject to medical necessity as determined by the Plan. All out-of-network services are subject to reasonable and customary (R&C) limitations. EPO Plan The Plan will pay the designated percentage of covered charges if the provider is in the EPO network until out-of-pocket amounts are reached, at which time the Plan will pay 100% of the remainder of covered charges for the rest of the calendar year unless stated otherwise. The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%: deductible(s), cost containment penalties, and above usual and customary charges. There is no out-of-network coverage under the EPO Plan unless otherwise required by law. EPO PLAN FMOLHS EPO NETWORK OUT-OF-NETWORK ANNUAL DEDUCTIBLE EMPLOYEE ONLY $250 No Coverage EMPLOYEE WITH DEPENDENTS $500 No Coverage MAXIMUM OUT-OF-POCKET (INCLUDES DEDUCTIBLE) EMPLOYEE ONLY $2,000 No Coverage EMPLOYEE WITH DEPENDENTS $4,000 No Coverage OFFICE VISIT PRIMARY CARE PHYSICIAN (PCP) $0 copay No Coverage SPECIALIST $35 copay No Coverage EMERGENCY ROOM/URGENT CARE EMERGENCY ROOM $250 copay $250 copay URGENT CARE $60 copay No Coverage OTHER COPAYS OUTPATIENT SURGERY $250 copay No Coverage INPATIENT $200 copay per day (4 day/$800 max) No Coverage PHYSICIAN SERVICES INPATIENT VISITS Included in Inpatient copay No Coverage Included in Of昀椀ce Visit copay, Outpatient Surgery OUTPATIENT copay, or 100% coverage after deductible No Coverage (depending on place of service) HOSPITAL SERVICES ROOM AND BOARD Included in Inpatient copay No Coverage INTENSIVE CARE UNIT Included in Inpatient copay No Coverage OUTPATIENT SURGERY Included in outpatient surgery copay No Coverage SKILLED NURSING FACILITY $200 copay per day (4 day/$800 max) No Coverage BARIATRIC SURGERY Plan Coverage for Bariatric surgery is available only to a Full-Time $3,000 copay; Surgery must be performed or Part-Time Active employee who is a Class A Participant who No Coverage remains in that status on the date of service and satis昀椀es the at a MBSAQIP Accredited FMOLHS facility requirements in Exhibit C and employee’s covered spouse and dependent who satis昀椀es the requirements in Exhibit C. ORGAN TRANSPLANT 90% coverage after deductible when performed No Coverage Blue Distinction Centers coverage only. at Blue Distinction Center facility OTHER SERVICES ALLERGY TESTING 90% coverage after deductible or included in of昀椀ce visit No Coverage copay, depending on place of service ALLERGY SERUM AND INJECTIONS 90% coverage after deductible or included in of昀椀ce visit No Coverage copay, depending on place of service OTHER INJECTIONS 90% coverage after deductible or included in of昀椀ce visit copay, depending on place of service 17
EPO PLAN (CONTINUED) FMOLHS EPO NETWORK OUT-OF-NETWORK OTHER SERVICES 90% coverage after deductible or included in of昀椀ce visit DIAGNOSTICS No Coverage copay, depending on place of service 90% coverage after deductible or included in of昀椀ce visit LABORATORY No Coverage copay, depending on place of service 90% coverage after deductible or included in of昀椀ce visit CHEMOTHERAPY No Coverage copay, depending on place of service 90% coverage after deductible; limited to 50 visits HOME HEALTH CARE No Coverage per calendar year HOSPICE CARE 90% coverage after deductible No Coverage AMBULANCE SERVICE 90% coverage after deductible No Coverage OCCUPATIONAL THERAPY 90% coverage after deductible; maximum of 120 visits PHYSICAL THERAPY per year (and maximum of 20 visits per week) combined No Coverage SPEECH THERAPY Occupational, Physical, and Speech Therapy 90% coverage after deductible maximum of APPLIED BEHAVIOR ANALYSIS (ABA) No Coverage 20 hours per week annually SPECIFIC GENETIC TESTING 90% coverage after deductible drawn/ordered by (MUST SATISFY MEDICALLY NECESSARY CRITERIA) FMOLHS Geneticist No Coverage 100% coverage of screening for tobacco use and two SMOKING CESSATION AIDS tobacco cessation attempts per year which includes four tobacco cessation counseling sessions of at least Smoking cessation is available through the No Coverage 10 minutes each without prior authorization and 90 day prescription bene昀椀t program. supply of Smoking Cessation Aids when prescribed by a health care provider without prior authorization DURABLE MEDICAL EQUIPMENT (DME) 90% coverage after deductible No Coverage INSULIN PUMP 90% coverage after deductible; limited to 1 per 5 years No Coverage ORTHOTICS AND PROSTHETICS 90% coverage after deductible No Coverage GENERIC DIABETES PRESCRIPTION 100% coverage of Generic Diabetes Prescription MEDICATIONS AND SUPPLIES Medications and Preferred Supplies through the No coverage pharmacy bene昀椀t. MENTAL HEALTH AND SUBSTANCE ABUSE INPATIENT INCLUDING PARTIAL HOSPITALIZATION (PHP), INTENSIVE $200 copay per day (4 day/$800 max) No Coverage OUTPATIENT PROGRAM (IOP), AND RESIDENTIAL OFFICE VISIT $0 Copay No Coverage 90% coverage after deductible or included in of昀椀ce visit OTHER OUTPATIENT SERVICES No Coverage copay, depending on place of service PREGNANCY CARE AND DELIVERY LABOR & DELIVERY AND ASSOCIATED CHARGES $200 copay per day (4 day/$800 max) No Coverage 90% coverage after deductible or included in of昀椀ce visit MATERNAL/FETAL ULTRASOUND copay, depending on place of service and other than No Coverage included in prenatal care IN NETWORK BREAST PUMP AND LACTATION COUNSELING THROUGH HEALTHY LIVES 100% coverage No Coverage One-time $50 copay applies for coverage of routine PRE-NATAL CARE OB visits, initial routine labs and one ultrasound No Coverage per term pregnancy. PREVENTIVE CARE ROUTINE WELL ADULT CARE Generally limited to approved preventive or wellness services, which could include the following annual screenings depending 100% coverage on your age, gender, and health status: Lipid (Cholesterol), HGB Limited to one routine physical examination No Coverage A1C (Diabetes), Bone Marrow Density Test, Mammogram, Pap annually and approved wellness screenings annually Test, Fecal Occult Blood Test, Colonoscopy, Depression Screening, Obesity Screening and Counseling. *Please call the Claims Administrator to con昀椀rm coverage ADULT IMMUNIZATIONS 100% coverage No Coverage Immunizations are subject to current CDC Recommendations which include age limitations ROUTINE WELL CHILD CARE Unlimited routine of昀椀ce visits through age two (2); annually ages 100% coverage No Coverage three (3) up. Includes: of昀椀ce visits, routine physical examination and immunizations in accordance with CDC Guidelines and preventive care in accordance with federal guidelines. *FMOLHS follows federal guidelines for coverage of preventive/wellness screenings. 18
PPO Plan The Plan will pay the designated percentage of covered charges until out-of-pocket amounts are reached, at which time the Plan will pay 100% of the remainder of covered charges for the rest of the calendar year unless stated otherwise. The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%: deductible(s), cost containment penalties, and above usual and customary charges. PPO PLAN FMOLHS NETWORK PREFERRED PROVIDER NON-PREFERRED OUT-OF-NETWORK (TIER 1) NETWORK (TIER 2) PROVIDER (TIER 3) ANNUAL DEDUCTIBLE EMPLOYEE ONLY $800 $800 $3,000 $5,000 EMPLOYEE WITH DEPENDENTS $1,600 $1,600 $6,000 $10,000 MAXIMUM OUT-OF-POCKET (INCLUDES DEDUCTIBLE) EMPLOYEE ONLY $3,000 $4,000 $6,000 $10,000 EMPLOYEE WITH DEPENDENTS $6,000 $8,000 $12,000 $20,000 Out of Area Coverage. A subscriber (team member) who is enrolled in the PPO Plan and whose home address is in a state other than Louisiana or Mississippi may (i) access care at Tier 2 network coverage with a BCBS PPO network provider in their home state for themselves and their enrolled dependents or (ii) access providers in the FMOLHS Louisiana and Mississippi networks at Tier 1 or Tier 2 coverage. Any other network access would follow the Tier 3 or Out-of-Network coverage. The Out of Area Coverage is based solely on the subscriber’s (team member’s) home address. A dependent’s address does not entitle the dependent to Out of Area Coverage. OFFICE VISIT $5 copay of昀椀ce visit only, $30 copay of昀椀ce visit only, PCP/MEDICAL HOME all other services subject to all other services subject to deductible and coinsurance deductible and coinsurance 60% coverage 40% coverage after deductible after deductible $45 copay of昀椀ce visit only, $70 copay of昀椀ce visit only, SPECIALIST all other services subject to all other services subject to deductible and coinsurance deductible and coinsurance EMERGENCY ROOM/URGENT CARE EMERGENCY ROOM 80% coverage after deductible URGENT CARE $75 copay $75 copay 60% coverage after deductible 40% coverage PHYSICIAN SERVICES INPATIENT VISITS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible OUTPATIENT 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible HOSPITAL SERVICES ROOM AND BOARD 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible INTENSIVE CARE UNIT 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible SURGERY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible SKILLED NURSING FACILITY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible BARIATRIC SURGERY Plan Coverage for Bariatric surgery is available only to a Full-Time or Part-Time Active $3,000 copay; Surgery must employee who is a Class A Participant who be performed at a MBSAQIP No coverage No coverage No coverage remains in that status on the date of service Accredited FMOLHS facility and satis昀椀es the requirements in Exhibit C and employee’s covered spouse and dependent who satis昀椀es the requirements in Exhibit C ORGAN TRANSPLANT 80% coverage after deductible No coverage Blue Distinction Centers coverage only. when performed at Blue Distinction Center facility OTHER SERVICES ALLERGY TESTING 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible ALLERGY SERUM AND INJECTIONS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible OTHER INJECTIONS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible DIAGNOSTICS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible LABORATORY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible CHEMOTHERAPY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible 80% coverage after deductible; 70% coverage after deductible; 60% coverage after deductible; HOME HEALTH CARE maximum of 50 visits per maximum of 50 visits per maximum of 50 visits per No coverage calendar year calendar year calendar year HOSPICE CARE 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible AMBULANCE SERVICE 80% coverage after deductible 19
PPO PLAN (CONTINUED) FMOLHS NETWORK PREFERRED PROVIDER NON-PREFERRED OUT-OF-NETWORK (TIER 1) NETWORK (TIER 2) PROVIDER (TIER 3) OTHER SERVICES OCCUPATIONAL THERAPY 80% coverage after deductible; 70% coverage after deductible 60% coverage after deductible PHYSICAL THERAPY No coverage SPEECH THERAPY Maximum of 120 visits per year (and maximum of 20 visits per week) combined with Occupational, Physical, and Speech Therapy 70% coverage after deductible; 80% coverage after deductible; 60% coverage after deductible; APPLIED BEHAVIOR ANALYSIS (ABA) No coverage max 20 hours per week annually max 20 hours per week annually max 20 hours per week annually SPECIFIC GENETIC TESTING 80%; drawn/ordered by (MUST SATISFY MEDICALLY NECESSARY No coverage No coverage No coverage CRITERIA) FMOLHS Geneticist SMOKING CESSATION AID 100% coverage of screening for tobacco use and two tobacco cessation attempts per year which includes four tobacco cessation counseling sessions of at least 10 minutes each without prior authorization and No coverage Smoking cessation is available through the 90 day supply of Smoking Cessation Aids when prescribed by a health care provider without prior prescription bene昀椀t program authorization DURABLE MEDICAL EQUIPMENT (DME) 80% coverage after deductible; 70% coverage after deductible 60% coverage after deductible No coverage 80% coverage after deductible; 70% coverage after deductible; 60% coverage after deductible; INSULIN PUMP No coverage limited to 1 per 5 years limited to 1 per 5 years limited to 1 per 5 years ORTHOTICS AND PROSTHETICS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible GENERIC DIABETES 100% coverage of Generic Diabetes Prescription Medications PRESCRIPTION MEDICATIONS No coverage No coverage AND PREFERRED SUPPLIES and Preferred Supplies through the pharmacy bene昀椀t MENTAL/NERVOUS AND SUBSTANCE ABUSE INPATIENT Including Partial Hospitalization (PHP), 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible Intensive Outpatient Program (IOP) and Residential OFFICE VISIT ONLY $5 copay $30 copay 60% coverage after deductible 40% coverage after deductible OTHER OUTPATIENT SERVICES 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible PREGNANCY CARE AND DELIVERY LABOR & DELIVERY AND ASSOCIATED CHARGES 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible 80% coverage after deductible; 70% coverage after deductible; 60% coverage after deductible; MATERNAL/FETAL ULTRASOUND other than included in other than included in other than included in 40% coverage after deductible pre-natal care pre-natal care pre-natal care IN NETWORK BREAST PUMP AND LACTATION COUNSELING 100% coverage 100% coverage 100% coverage No coverage THROUGH HEALTHY LIVES One time $50 copay applies to routine OB visits, initial routine labs and PRE-NATAL CARE 40% coverage after deductible one ultrasound per term pregnancy. PREVENTATIVE CARE ROUTINE WELL ADULT CARE Generally limited to approved preventive or wellness services, which could include the 40% coverage 100% coverage 100% coverage 100% coverage following annual screenings depending on after deductible; Limited to one routine physical Limited to one routine physical Limited to one routine physical your age, gender, and health status: Lipid Limited to one routine physical examination annually and examination annually and examination annually and (Cholesterol), HGB A1C (Diabetes), Bone examination annually and Marrow Density Test, Mammogram, Pap approved wellness screenings approved wellness screenings approved wellness screenings approved wellness screenings Test, Fecal Occult Blood Test, Colonoscopy, annually. annually. annually. annually. Depression Screening, Obesity Screening and Counseling.* Please call the Claims Administrator to con昀椀rm coverage ADULT IMMUNIZATIONS Immunizations are subject to current CDC 100% coverage 100% coverage 100% coverage 40% coverage after deductible Recommendations which include age limitations ROUTINE WELL CHILD CARE Unlimited routine of昀椀ce visits through age two (2); annually ages three (3) up. Includes: 100% coverage 100% coverage 100% coverage 40% coverage after deductible of昀椀ce visits, routine physical examination and immunizations in accordance with CDC Guidelines and preventive care in accordance with federal guidelines. *FMOLHS follows federal guidelines for coverage of preventive wellness screenings. 20
HDHSA HDHSA Plan – A high deductible health plan with a tax-free health savings account (HSA). You determine how much you’ll contribute to the account, when to use the money to pay for quali昀椀ed medical, prescription, dental and vision services, and when to reimburse yourself. HSAs allow you to save and roll over money if you do not spend it in the calendar year. The money in this account is portable, even if you change plans or jobs. Company HSA contributions will be pro-rated based on enrollment date. You cannot open an HSA if: » You have other health coverage that helps you pay » You also have Medicare or TRICARE. for health care expenses before your deductible » Someone else can claim you as a dependent. is met. » You have used Veterans Affairs hospital or medical » You or your spouse has a 昀氀exible spending account services in the three months prior to opening your (FSA) or health reimbursement arrangement (HRA). HSA, unless it was for a disability related to your (You are allowed to participate in a Limited Use FSA, military service. which would only cover Dental and Vision expenses.) HIGH DEDUCTIBLE HSA PLAN FMOLHS NETWORK PREFERRED PROVIDER NON-PREFERRED OUT-OF-NETWORK (TIER 1) NETWORK (TIER 2) PROVIDER (TIER 3) HSA ANNUAL CONTRIBUTIONS EMPLOYEE ONLY $750 EMPLOYEE WITH DEPENDENTS $1,500 ANNUAL DEDUCTIBLE (AGGREGATED) EMPLOYEE ONLY $1,750 $1,750 $3,500 $4,000 EMPLOYEE WITH DEPENDENTS $3,500 $3,500 $7,000 $8,000 MAXIMUM OUT-OF-POCKET (INCLUDES DEDUCTIBLE) (EMBEDDED OOP) EMPLOYEE ONLY $3,500 $4,000 $7,000 $10,500 EMPLOYEE WITH DEPENDENTS $7,000 $8,000 $14,000 $21,000 The Out of Area coverage is not available under the High Deductible HSA Plan. OFFICE VISIT CHARGE ONLY PRIMARY CARE PHYSICIAN (PCP) 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible SPECIALIST 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible EMERGENCY ROOM/URGENT CARE EMERGENCY ROOM 80% coverage after deductible 80% coverage after deductible 80% coverage after deductible 80% coverage after deductible URGENT CARE 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible PHYSICIAN SERVICES INPATIENT VISITS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible OUTPATIENT 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible HOSPITAL SERVICES ROOM AND BOARD 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible INTENSIVE CARE UNIT 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible SURGERY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible SKILLED NURSING FACILITY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible 21
HDHSA PLAN (CONTINUED) FMOLHS NETWORK PREFERRED PROVIDER NON-PREFERRED OUT-OF-NETWORK (TIER 1) NETWORK (TIER 2) PROVIDER (TIER 3) HOSPITAL SERVICES BARIATRIC SURGERY Plan Coverage for Bariatric surgery is available only to a Full-Time or Part-Time Active $3,000 copay; Surgery must employee who is a Class A Participant who be performed at a MBSAQIP No coverage No coverage No coverage remains in that status on the date of service Accredited FMOLHS facility and satis昀椀es the requirements in Exhibit C and employee’s covered spouse and dependent who satis昀椀es the requirements in Exhibit C ORGAN TRANSPLANT 80% coverage after deductible No coverage Blue Distinction Centers coverage only when performed at Blue Distinction Center facility OTHER SERVICES ALLERGY TESTING 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible ALLERGY SERUM AND INJECTIONS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible OTHER INJECTIONS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible DIAGNOSTICS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible LABORATORY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible CHEMOTHERAPY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible 80% coverage after deductible; 70% coverage after deductible; 60% coverage after deductible; HOME HEALTH CARE maximum of 50 visits per maximum of 50 visits per maximum of 50 visits per No coverage calendar year calendar year calendar year HOSPICE CARE 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible AMBULANCE SERVICE 80% coverage after deductible OCCUPATIONAL THERAPY 80% coverage after deductible; 70% coverage after deductible 60% coverage after deductible PHYSICAL THERAPY No coverage SPEECH THERAPY Maximum of 120 visits per year (and maximum of 20 visits per week) combined with Occupational, Physical, and Speech Therapy 70% coverage after deductible; 80% coverage after deductible; 60% coverage after deductible; APPLIED BEHAVIOR ANALYSIS (ABA) No coverage max 20 hours per week annually max 20 hours per week annually max 20 hours per week annually SPECIFIC GENETIC TESTING 80%; drawn/ordered by (MUST SATISFY MEDICALLY NECESSARY No coverage No coverage No coverage CRITERIA) FMOLHS Geneticist SMOKING CESSATION AID 100% coverage of screening for tobacco use and two tobacco cessation attempts per year which includes four tobacco cessation counseling sessions of at least 10 minutes each without prior authorization and No coverage Smoking cessation is available through the 90 day supply of Smoking Cessation Aids when prescribed by a health care provider without prior prescription bene昀椀t program authorization DURABLE MEDICAL EQUIPMENT (DME) 80% coverage after deductible; 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible 80% coverage after deductible; 70% coverage after deductible; 60% coverage after deductible; INSULIN PUMP No coverage limited to 1 per 5 years limited to 1 per 5 years limited to 1 per 5 years ORTHOTICS AND PROSTHETICS 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible GENERIC DIABETES PRESCRIPTION MEDICATIONS 100% coverage of Generic Diabetes Prescription Medications No coverage No coverage AND PREFERRED SUPPLIES and Preferred Supplies through the pharmacy bene昀椀t Employee must satisfy deductible MENTAL/NERVOUS AND SUBSTANCE ABUSE INPATIENT Including Partial Hospitalization (PHP), 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible Intensive Outpatient Program (IOP) and Residential OFFICE VISIT ONLY 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible OTHER OUTPATIENT SERVICES 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible PREGNANCY CARE AND DELIVERY LABOR & DELIVERY AND ASSOCIATED CHARGES 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible MATERNAL/FETAL ULTRASOUND 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible 22
HDHSA PLAN (CONTINUED) FMOLHS NETWORK PREFERRED PROVIDER NON-PREFERRED OUT-OF-NETWORK (TIER 1) NETWORK (TIER 2) PROVIDER (TIER 3) PREGNANCY CARE AND DELIVERY IN-NETWORK BREAST PUMP AND LACTATION COUNSELING 100% coverage 100% coverage 100% coverage No coverage THROUGH HEALTHY LIVES PRE-NATAL CARE 80% coverage after deductible 70% coverage after deductible 60% coverage after deductible 40% coverage after deductible PREVENTATIVE CARE ROUTINE WELL ADULT CARE Generally limited to approved preventive or wellness services, which could include the 40% coverage 100% coverage 100% coverage 100% coverage following annual screenings depending on after deductible; Limited to one routine physical Limited to one routine physical Limited to one routine physical your age, gender, and health status: Lipid Limited to one routine physical examination annually and examination annually and examination annually and (Cholesterol), HGB A1C (Diabetes), Bone examination annually and Marrow Density Test, Mammogram, Pap approved wellness screenings approved wellness screenings approved wellness screenings approved wellness screenings Test, Fecal Occult Blood Test, Colonoscopy, annually. annually. annually. annually. Depression Screening, Obesity Screening and Counseling. *Please call the Claims Administrator to con昀椀rm coverage ADULT IMMUNIZATIONS Immunizations are subject to current CDC 100% coverage 100% coverage 100% coverage 40% coverage after deductible Recommendations which include age limitations ROUTINE WELL CHILD CARE Unlimited routine of昀椀ce visits through age two (2); annually ages three (3) up. Includes: 100% coverage 100% coverage 100% coverage 40% coverage after deductible of昀椀ce visits, routine physical examination and immunizations in accordance with CDC Guidelines and preventive care in accordance with federal guidelines. *FMOLHS follows federal guidelines for coverage of preventive wellness screenings. Note When you enroll in the HSA plan, PayFlex will provide you with a debit card that includes the FMOLHS annual contribution to help pay for eligible expenses. 23
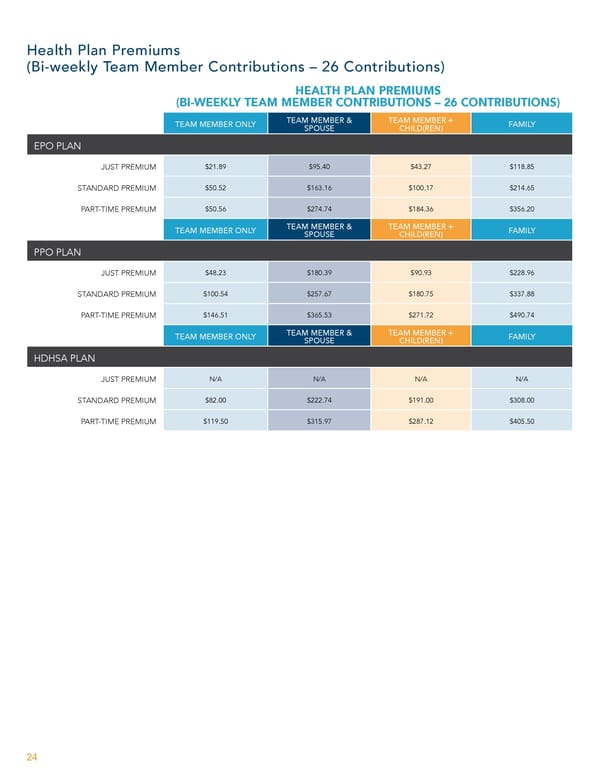
Health Plan Premiums (Bi-weekly Team Member Contributions – 26 Contributions) HEALTH PLAN PREMIUMS (BI-WEEKLY TEAM MEMBER CONTRIBUTIONS – 26 CONTRIBUTIONS) TEAM MEMBER & TEAM MEMBER + TEAM MEMBER ONLY FAMILY SPOUSE CHILD(REN) EPO PLAN JUST PREMIUM $21.89 $95.40 $43.27 $118.85 STANDARD PREMIUM $50.52 $163.16 $100.17 $214.65 PART-TIME PREMIUM $50.56 $274.74 $184.36 $356.20 TEAM MEMBER & TEAM MEMBER + TEAM MEMBER ONLY FAMILY SPOUSE CHILD(REN) PPO PLAN JUST PREMIUM $48.23 $180.39 $90.93 $228.96 STANDARD PREMIUM $100.54 $257.67 $180.75 $337.88 PART-TIME PREMIUM $146.51 $365.53 $271.72 $490.74 TEAM MEMBER & TEAM MEMBER + TEAM MEMBER ONLY FAMILY SPOUSE CHILD(REN) HDHSA PLAN JUST PREMIUM N/A N/A N/A N/A STANDARD PREMIUM $82.00 $222.74 $191.00 $308.00 PART-TIME PREMIUM $119.50 $315.97 $287.12 $405.50 24
This is a modal window.
My Pharmacy Bene昀椀ts Express Scripts (ESI) • www.express-scripts.com • 877-816-8717 Prescription Drug Coverage for Medical Plans Your prescription drug program will be coordinated through Express Scripts (ESI). Your cost is determined by the tier assigned to the prescription drug product. All prescription drug products on the prescription drug list (Express Scripts' National Preferred Formulary) are assigned as Generic, Preferred, Non-Preferred and Specialty. You may contact ESI for information on your bene昀椀t coverage and search for network pharmacies by logging on to www.express-scripts.com or calling ESI Customer Care at 877-816-8717. Why Do My Prescriptions Cost So Much? In recent years, drug costs have increased, outpacing in昀氀ation by nearly four times annually. Rising drug costs are one of the single largest causes of the ballooning cost of health care. Although rising drug costs are inevitable, there are many ways you, the patient, with the help of your physician, can minimize your prescription drug costs while maintaining the same quality of health. You share the cost of your medications with your employer. Your share of the cost is called a copay or coinsurance. Some plans offer lower copays for less costly drugs. For example, they charge one copay for a Generic drug, a higher copay for a Preferred drug, and an even higher copay for a Non-Preferred drug. Coinsurance is a percent of the drug’s cost. When you pay a percentage, your cost may be high for many reasons: » The cost of the drug may be high. Let’s assume your coinsurance is 20%. In this case, a $250 drug will be more costly than a $25 drug. » Your drug may not be on the Preferred Drug List, so you pay at a higher tier. » You may be buying a more expensive brand-name drug when there is a generic equivalent available for less money. How Can I Minimize My Medication Costs? » Consider Mail Order for your maintenance medications. You receive a 3-month supply for only two copays if you 昀椀ll your prescription at RxONE. Example: EPO PLAN ANNUAL COST PRESCRIPTION GENERIC – IN-HOUSE $10 per month $120 GENERIC – MAIL ORDER $20 per 3 months $80 YOUR ANNUAL SAVINGS N/A $40 » You can explore the bene昀椀ts available to you before enrolling by visiting https://www.express-scripts.com/fmolhs. Here you can review plan options, 昀椀nd prices on medications under the plan, and explore an overview of the bene昀椀ts offered. » Print a copy of the Express Scripts National Preferred formulary and bring it with you when you visit your physician. Log on to www.express-scripts.com, and click on Register. Once you complete the registration you will have access to your account information, bene昀椀ts and formulary list. » Let your physician know that you would like to try generics 昀椀rst, if that is an appropriate option for you. » Ask your provider if there are Over-the-Counter (OTC) products available to obtain the same results as prescription medications. Often these OTC products will be less expensive than your copay and will provide the same relief. » Get a $5 discount when you 昀椀ll your prescription at an in-house pharmacy. Get an additional $5 discount when your prescription is written by the Franciscan Clinic and 昀椀lled at the in-house pharmacy. Refer to page 27 for a listing of the in-house pharmacy locations/services. 25
EPO PRESCRIPTION PLAN COST IN-HOUSE NETWORK RETAIL PHARMACY (30-DAY SUPPLY) GENERIC DRUG $10 copay $15 copay GENERIC DIABETIC PRESCRIPTION MEDICATIONS AND SUPPLIES $0 copay $0 copay PREFERRED DRUG $35 copay $70 copay NON-PREFERRED DRUG $70 copay $110 copay SPECIALTY DRUG Filled by RxONE – $100 copay Filled by Express Scripts – $150 copay MAIL ORDER PHARMACY (90-DAY SUPPLY — RXONE OR EXPRESS SCRIPTS) GENERIC DRUG PREFERRED DRUG 2x in-house copay* 3x network copay* NON-PREFERRED DRUG BRAND-NAME DRUGS WHEN GENERIC IS AVAILABLE The brand copayment, plus the difference between the retail cost of the brand-name drug and of the generic drug. Note: The difference will not be applied to the out-of-pocket maximum. IMMUNIZATIONS According to CDC Immunization Schedules; Subject to age limitations *Mail order copays do not apply to mail order Specialty Prescriptions. PPO PRESCRIPTION PLAN COST IN-HOUSE NETWORK RETAIL PHARMACY (30-DAY SUPPLY) GENERIC DRUG $10 copay $15 copay GENERIC DIABETIC PRESCRIPTION MEDICATIONS AND SUPPLIES $0 copay $0 copay PREFERRED DRUG $45 copay $70 copay NON-PREFERRED DRUG $70 copay $110 copay SPECIALTY DRUG Filled by RxONE – $100 copay Filled by Express Scripts – $150 copay MAIL ORDER PHARMACY (90-DAY SUPPLY – RXONE OR EXPRESS SCRIPTS) GENERIC DRUG PREFERRED DRUG 2x In-house copay* 3x Network copay* NON-PREFERRED DRUG BRAND-NAME DRUGS WHEN GENERIC IS AVAILABLE The brand copayment, plus the difference between the retail cost of the brand-name drug and of the generic drug. Note: The difference will not be applied to the out-of-pocket maximum. IMMUNIZATIONS According to CDC Immunization Schedules; Subject to age limitations *Mail order copays do not apply to mail order Specialty Prescriptions. 26
HDHSA PRESCRIPTION PLAN COST IN-HOUSE NETWORK RETAIL PHARMACY (30-DAY SUPPLY) GENERIC DRUG 20% after deductible 20% after deductible GENERIC DIABETIC PRESCRIPTION MEDICATIONS AND SUPPLIES 20% after deductible 20% after deductible PREFERRED DRUG 20% after deductible 20% after deductible NON-PREFERRED DRUG 20% after deductible 20% after deductible SPECIALTY DRUG (RXONE OR EXPRESS SCRIPTS) 20% after deductible 20% after deductible MAIL ORDER PHARMACY (90-DAY SUPPLY — RXONE OR EXPRESS SCRIPTS) GENERIC DRUG PREFERRED DRUG 20% after deductible NON-PREFERRED DRUG BRAND-NAME DRUGS WHEN GENERIC IS AVAILABLE The brand copayment, plus the difference between the retail cost of the brand-name drug and of the generic drug. Note: The difference will not be applied to the out-of-pocket maximum. IMMUNIZATIONS According to CDC Immunization Schedules; Subject to age limitations *Mail order copays do not apply to mail order Specialty Prescriptions. IN-HOUSE PHARMACY OVERVIEW SERVICES SERVICE PHARMACY LOCATION EMPLOYEE AREA FLAVOR- MAIL IMMUNI- RETAIL SPECIALTY DELIVERY HEALTHPLAN ING ORDER ZATIONS DISCOUNT * 1014 West St. Claire Blvd Ste. 1010 RxONE | Ascension LA 225-271-6098 7777 Hennessy Blvd Ste 114, BR RxONE | Med Plaza LA 225-765-8951 5000 Hennessy, Chapel Hallway Rm 101, BR RxONE| Lake LA 225-374-0260 2600 Tower Dr., Monroe RxONE | Tower Drive LA 318-966-6290 309 Jackson St, Monroe RxONE | St Francis LA & MS MS only 318-966-7242 4809 Ambassador Caffery Pkwy, Laf RxONE | Lourdes 337-470-4342 LA & MS MS only 5131 O’Donovan Dr, BR O'Donovan Pharmacy 225-374-0270 LA 1401 N. Foster Dr, BR Mid City Pharmacy LA 225-987-9184 8300 Constantin Blvd, BR Lake Children's Pharmacy LA 225-374-1350 433 Plaza St., Bogalusa, LA Our Lady of the Angel OP LA 985-730-7219 27
Preauthorization Requirement List Note: The following services, supplies and care must be preauthorized or reimbursement from the Plan may be reduced. To preauthorize services, your provider can contact Blue Cross Blue Shield at 833-468-3594. If preauthorization requirements are not met, covered expenses will be paid at 50% if the services are Medically Necessary and 0% if the services are not Medically Necessary. If you have any questions regarding medical preauthorization, call Blue Cross Blue Shield at 833-468-3594. » All Inpatient Admissions (Includes acute, Skilled, » Growth Hormones Rehabilitation, LTAC and Treatment Room Services) » Home Health » All Clinical Trials, Experimental & Investigational » Hyperbaric Oxygen Therapy Procedures/Treatment » Injectables (Boniva, Reclast, Hyalgan, Synagis, » All Transplant Services Including Pre-Transplant Orthovisc, Supartz, Botox, & Growth Hormones) Evaluations » Insulin Pump » All Out-of-Network and Out-of-Area Services, except » IV Infusions inpatient admissions, outpatient services, residential » Mental Health Services treatment, home health and hospice » All Plastic & Reconstructive Surgeries & Procedures » Orthotics and Prosthetics over $1,000 (with the exception of fracture or sprain diagnosis) (Cosmetic procedures are excluded from coverage) » All CT Scans and MRIs including CTAs and MRAs » PET Scans » 17 Alpha-Hydroxyprogesterone Caproate (17P) » Pain Management procedures » Alcohol/Substance Abuse » Podiatry treatment » Applied Behavior Analysis » Diagnostic studies and/or treatment of Sleep » Bariatric Surgery Disorders » Diabetic Education » Surgery (hysterectomy, varicose vein, nasal/septal » Durable Medical Equipment (purchases over $500 surgery, breast reduction, surgical intervention to correct sleep apnea, oral surgery) and all rentals) » Therapies – Physical, Speech, Occupational » Enteral Feedings » Non-Emergent Air Ambulance and Non-Emergent » Epidural Steroid Injections Ambulance Transportation » Genetic Studies/Testing/Therapy » Weight Loss Program & Medications (This list is not inclusive of all codes requiring prior authorizations; please contact Member Services for bene昀椀ts, eligibility, and code speci昀椀c requirements at 833-468-3594.) 28
Which Preventive Services Can I Get With No Out-of-Pocket Expenses? Depending on your age, you may have access at reduced or no cost to such preventive services as: » One adult routine preventive care visit annually: » Blood pressure, diabetes, and cholesterol tests; » Screening tests for many common types of cancers, including mammograms and colonoscopies (the test used to screen for colon cancer) in accordance with U.S. Preventive Services Task Force (USPSTF) recommendations; » Counseling from your health care provider on such topics as quitting smoking, losing weight, eating healthy, treating depression, and reducing alcohol use; » Routine vaccinations against disease, such as measles, polio, meningitis, 昀氀u and pneumonia shots in accordance with CDC recommendations; » Counseling, screening, and vaccines to ensure healthy pregnancies; and » Regular well-baby and well child visits from birth to age 21. Screening in these areas (blood pressure, cholesterol, glucose, obesity) can be completed by scheduling your annual well visit with your Primacy Care Provider. Note For a complete list of affected preventive services, go to www.healthcare.gov/coverage/preventive-care-bene昀椀ts/ 29
2023 ADULT PREVENTIVE SERVICE RECOMMENDATIONS¹ THIS CHART IS INTENDED AS A REFERENCE TOOL FOR YOUR CONVENIENCE. AGE 21-39 40-49 50-64 65 or older PREVENTION/SCREENING One time screening by ABDOMINAL AORTIC ANEURYSM SCREENING ultrasonography in men ages 65-75 who have ever smoked BREAST CANCER SCREENING As recommended Screening mammography, every year, for by your health care women age 40 years and older, with or without (BRCA²; MEDICATION³) provider* clinical breast examination Cytology (Pap smear) every 3 years women ages 21 – 65 or As recommended CERVICAL CANCER SCREENING by your health care Ages 30 – 65 years who want to lengthen the interval, screening with a provider* combination of cytology & human papillomavirus (HPV) testing every 5 yrs. Men ages 20 – 35 for lipid disorders if they are at increased risk for CHOLESTEROL ABNORMALITIES SCREENING: MEN coronary heart disease Men ages 35 and older for lipid disorders Women ages 30 – 45 years for lipid disorders if they CHOLESTEROL ABNORMALITIES are at increased risk for coronary heart disease SCREENING: WOMEN Women age 45 years and older for lipid disorders As recommended by your Adults beginning at age 45, fecal occult blood COLORECTAL CANCER SCREENING testing annually, sigmoidoscopy every 5 years, or health care provider* colonoscopy every 10 years DIABETES SCREENING Beginning at age 45 (If you have high blood pressure or high cholesterol, are overweight, or have a close family history of diabetes, you should consider an earlier screening.) HEPATITIS C SCREENING Adults age 18 – 79 without known liver disease, a one-time screening for hepatitis C virus (HCV) 4 IMMUNIZATIONS Refer to the CDC’s posted schedule of immunizations LUNG CANCER SCREENING Annual screening with low-dose computed Screening should be discontinued once a person has not tomography in adults age 50 – 80 years who have a smoked for 15 years or develops a health problem that substantially limits life expectancy or the ability or 20 pack-year smoking history and currently smoke or have quit within the past 15 years. willingness to have curative lung surgery OSTEOPOROSIS SCREENING Bone density in younger women whose fracture risk is equal to or greater than Bone density for women that of a 65 year old white woman who has no additional risk factors. age 65 years or older WELLNESS OFFICE VISIT: PHYSICAL EXAM, BLOOD PRESSURE, BODY MASS INDEX (BMI) Annually * High Risk: There is no age limit for screening if you are at high risk: Colon cancer: If you or a close relative had colorectal polyps or colorectal cancer or if you have in昀氀ammatory bowel disease. Breast cancer: This might include women who carry genes that increase their risk of breast cancer, such as the “BRCA” genes or who have close relatives who were diagnosed with breast cancer at a young age. ¹ https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics (current as of June 2022) ² BRCA risk assessment and genetic counseling/testing: Screen women whose family history may be associated with an increased risk for potentially harmful BRCA mutations. Women with positive screening results should receive genetic counseling and, if indicated after counseling, BRCA testing. ³ Breast cancer preventive medications: Asymptomatic women aged ≥35 years without a prior diagnosis of breast cancer who are at increased risk for the disease. Clinicians engage in shared, informed decision making with women who are at increased risk for breast cancer about medications to reduce their risk. 4 Adult immunizations: https://www.cdc.gov/vaccines/schedules/index.html Additional preventive care bene昀椀ts may be covered under the health plan. 30
Care Management In partnership with your primary care provider, you have access to additional resources to meet your health goals. A care team will work closely with physicians to provide the care needed for individuals with chronic diseases such as diabetes, high blood pressure, heart failure and asthma. The entire care team will work together to provide seamless care, will help individuals navigate the health care system and get connected with the resources needed to better manage their disease. Below are a couple of the focus areas and the bene昀椀ts available for health plan members who qualify: Transition Care Targets patients who are discharged from the hospital and have previously been identi昀椀ed as having a high likelihood of readmission within 30 days. Complex Care Targets patients who are living with complex chronic conditions, such as hypertension and diabetes, and are at high risk for either an emergency or inpatient encounter. Diabetes Management Program Disease management is a con昀椀dential program provided by FMOLHS to help you or a covered dependent living with a chronic condition. Diabetes coaching is available through Healthy Lives. Eligible team members and dependents will have access to a personal health coach and together develop achievable goals and strategies for improving their overall health. When you work with a nurse coach, you’ll get tips and practical tools for managing your chronic condition. They will also help you set up a plan to reach personal goals. Coaching is a great way to re-energize yourself to improve or manage your condition. Maternity Management In partnership with your health care provider, a Healthy Lives registered nurse will assist you throughout your pregnancy with your personalized health needs. Maternity management nurses will have personal contact each trimester and provide 昀椀rst year of life education. Individuals engaged in maternity management receive free preconception counseling and prenatal information. 31
My Health and Well-Being To participate in the 2023 Health and Wellness Program My Health and Well-being Program Now more than ever we recognize the importance and to begin earning points, follow the steps below: 1. Complete your HRA Questionnaire on the Healthy of offering opportunities to care for your health and Lives app or web-based portal. well-being. Our well-being program provides you with a more streamlined and personalized program and gives 2. Schedule and complete your wellness visit with you more opportunities to engage and get rewarded for your PCP between December 16, 2022 and participating in health and well-being activities. December 15, 2023. During your wellness visit, your PCP will perform your annual wellness exam Your primary care physician (PCP) should be your main point and your biometric screening. of contact in your wellness journey. You’ll have to complete this PCP visit along with completing the HRA questionnaire – NOTE: Contact our Network Guides at to be eligible for rewards under the well-being program. 855-875-6265 if you need assistance 昀椀nding Each point you earn equals $1 in rewards. Team members a primary care provider or scheduling an can earn up to 550 points or $550 in rewards.* appointment. You have many options on how to redeem points that you 3. Engage in approved activities that help you achieve earn. We have partnered with a company called Awardco, your goals and earn your rewards. which will enable you to redeem your wellness points – There is a catalog of approved activities available on things such as Amazon items, hotels, virtual pre-paid on the Total Rewards site on the My Health and cards, e-gift cards, movie tickets, or cash the rewards Well-being page or on the Healthy Lives portal. out for additional money on your paycheck. The choice is yours! Earned points will be available for redemption Review the activities and determine which best 昀椀t with your work-life schedule and complete the on the 15th of each month. activities. Then follow the steps to con昀椀rm your participation in the activities. 4. Redeem your points for rewards of your choice on the Awardco site, which can be accessed through the Healthy Lives portal or online at https://fmolhs.awardco.com. You will need to register on the Awardco site to access your rewards. *Maximum annual rewards are prorated based on employment status: Full time 100%, part-time 50% and PRN 25%. To receive the reward, the team member must Note be actively employed on the date of the reward payment. Reward payments are subject to state and federal taxes. For questions about the Well-being Program, In addition to completing your wellness visit with your please contact Healthy Lives at 855-426-4325 PCP, you can work with our partner, Healthy Lives, and or visit www.ourhealthylives.org. You can also meet with a personal health coach to review your wellness get additional information by visiting our Total screening results, create a personal plan to help you Rewards site at fmolhs.org/totalrewards on the reach your health and well-being goals, and earn rewards for doing so. My Health and Well-being page. 32
Healthy Lives • www.ourhealthylives.org • 855-426-4325 Your medical information is private and protected. Your participation in the Healthy Lives Wellness program is your personal choice. The results of your screening and personal wellness plan are not shared with your employer. work environment that wants you to succeed. Timely health Healthy Lives Wellness Program topics are delivered via live remote presentations, podcasts, Working well begins with living well. We’re pleased in-person seminars and more. Everything is at your 昀椀ngertips to be a partner for your personal health journey. As a through the mobile Healthy Lives app to help you keep track bene昀椀t to every team member, we offer the Healthy Lives of your progress, review health and well-being activities Wellness Program to support and encourage individual to earn wellness points, and schedule the education that’s health goals. All team members can participate at no important to you. Your coach will make suggestions too! Here cost. Whether at home or work, these tools and personal are some of the options offered: coaching help each team member and their family Health identify what’s important to their health and well-being Wellness Classes Walking Groups Tobacco Cessation Coaching with a plan to achieve results. Body, mind and spirit – our Pregnancy Farm To Work Stretch Breaks Meal Planning wellness approach is comprehensive and complements Program your personal physician's care and personal health goals. Stress Diabetes Team Challenges Nutrition Education Management Prevention Personal Coaching and Kinesics Continual Education Kinesics is a platform to improve balance and mobility that is personalized to address your individual needs. Once the wellness visit and biometric screening are complete Schedule through the Healthy Lives app/portal, and with your PCP, schedule a one-on-one health coaching you will receive a full range of motion evaluation and session with Healthy Lives, Your health coach will explain the a one-on-one results review. Team members receive a screening results and create a personal plan to help you reach customized 昀氀exibility and mobility program that is 100% your health goals. You’ll be surrounded and supported by a unique to your body and includes video tutorials, so you feel con昀椀dent about executing your program. Healthy Lives Wellness App Take your plan and your progress with you everywhere using the mobile app. This interactive tool helps you keep track of total well-being and manage your healthy lifestyle choices. Through this mobile tracker, you’ll also stay connected to all of the Healthy Lives Wellness resources, including chats with a health coach. The app is free to download and compatible with all mobile devices. To learn more about the Health and Wellness Program and Healthy Lives, visit www.OurHealthyLives.org or call 855-426-4325 for Louisiana ministries or 601-200-6448 for Mississippi ministries. 33
In addition, all medical information obtained through the wellness program Notice Regarding will be maintained separate from your personnel records, information stored electronically will be encrypted, and no information you provide as part of the wellness program will be used in making any employment decision. Appropriate Wellness Program precautions will be taken to avoid any data breach, and in the event a data breach occurs involving information you provide in connection with the wellness Healthy Lives is a voluntary wellness program available to both health plan and program, we will notify you immediately. non‑health plan members. The program is administered according to federal You may not be discriminated against in employment because of the medical rules permitting employer‑sponsored wellness programs that seek to improve information you provide as part of participating in the wellness program, nor may employee health or prevent disease, including the Americans with Disabilities Act you be subjected to retaliation if you choose not to participate. of 1990, the Genetic Information Nondiscrimination Act of 2008, and the Health Insurance Portability and Accountability Act, as applicable, among others. If you If you have questions or concerns regarding this notice, or about protections choose to participate in the wellness program you will be asked to complete a against discrimination and retaliation, please contact Human Resources. voluntary health risk assessment or “HRA” that asks a series of questions about your health‑related activities and behaviors and whether you have or had certain medical conditions (e.g., cancer, diabetes, or heart disease). You will also be asked to complete a biometric screening, which will include a blood test for total cholesterol, HDL, LDL, triglycerides and glucose (include cotinine screening, if appropriate). Your blood pressure, height, weight, and waist circumference will also be measured. You are not required to complete the HRA or to participate in the blood test or other medical examinations. Incentives may be available for employees who participate in certain health‑related activities or achieve certain health outcomes. If you are unable to participate in any of the health‑related activities or achieve any of the health outcomes required to earn an incentive, you may be entitled to a reasonable accommodation or an alternative standard. You may request a reasonable accommodation or an alternative standard by contacting Healthy Lives at 855‑426‑4325. The information from your HRA and the results from your biometric screening will be used to provide you with information to help you understand your current health and potential risks, and may also be used to offer you services through the wellness program, such as wellness programming and content. You also are encouraged to share your results or concerns with your own doctor. Protections from Disclosure of Medical Information We are required by law to maintain the privacy and security of your personally identi昀椀able health information. Although the wellness program and FMOLHS may use aggregate information it collects to design a program based on identi昀椀ed health risks in the workplace, Healthy Lives will never disclose any of your personal information either publicly or to the employer, except as necessary to respond to a request from you for a reasonable accommodation needed to participate in the wellness program, or as expressly permitted by law. Medical information that personally identi昀椀es you that is provided in connection with the wellness program will not be provided to your supervisors or managers and may never be used to make decisions regarding your employment. Your health information will not be sold, exchanged, transferred, or otherwise disclosed except to the extent permitted by law to carry out speci昀椀c activities related to the wellness program, and you will not be asked or required to waive the con昀椀dentiality of your health information as a condition of participating in the wellness program or receiving an incentive. Anyone who receives your information for purposes of providing you services as part of the wellness program will abide by the same con昀椀dentiality requirements. In order to provide you with services under the wellness program, your personally identi昀椀able health information may be shared with one or more of the following: Mercer, Lockton Companies, Blue Cross Blue Shield, Express Scripts (ESI) and Health Leaders Network. 34
My Dental Bene昀椀ts Delta Dental www.deltadentalins.com • 800-521-2651 Diagnostic and Preventive Care Services will no longer Choose a PPO Dentist to Save! accrue towards your plan year maximums. This includes The dental plan allows a participant to visit any licensed x-rays, cleanings and exams. dentist, but by taking advantage of the nationwide PPO Proper dental care plays an important role in your overall network you will maximize the value of the plan. You can good health. Our Dental Plan is designed to encourage search the Delta Dental PPO Network for a dentist near preventive treatment, allowing team members to achieve you by visiting http://www.deltadentalins.com/dentist- oral health while striving to minimize dental costs. The Dental directory/ppo.html. Plan will be administered by Delta Dental. Enrolled team members will also have access to hearing aid discounts. Delta Dental Delta Dental Non-Delta ® PPO Premier Dental 1. Greater Savings 4. Avoid Unbundling PPO dentists have agreed to reduce fees, which PPO dentists agree to not unbundle services that are part leaves more money in your pocket. of a treatment. Out-of-Network dentists may charge for these services separately, making the overall cost higher. 2. Quality Assurance 5. Less Paperwork Delta monitors PPO dentists to ensure that proper licensing, cleanliness and safety procedures are followed PPO dentists handle all claim forms and other paperwork for and send regular updates on policies and contracting you. If you choose an out-of-network dentist, you may be requirements. required to submit the claim yourself. 3. No Balance Billing 6. No Prepayment Required PPO dentists cannot charge you more than their set When you choose a PPO dentist, you will pay only your fees. Out-of-Network dentists may bill the difference portion of the bill. Out-of-Network dentists may require you between their usual feel and Delta Dental’s contracted to pay up front and request a reimbursement from Delta rate — a process known as “balance billing”. Dental when the claim is submitted. Note While you may seek services covered under the Dental Plan from any dentist, you will have access to discounted pricing when utilizing the PPO network dentists. 35
Dental Premiums Dental premium contributions will be deducted from your paycheck on a before-tax basis. Your tier of coverage will determine your semi-monthly premiums (24 deductions). BASIC PLAN BUY UP PLAN FULL TIME PART TIME FULL TIME PART TIME 2023 PREMIUMS TEAM MEMBER $3.90 $7.80 $7.92 $15.83 TEAM MEMBER + FAMILY $24.50 $28.40 $36.15 $44.07 Dental Plan Coverage DENTAL PLAN BASIC PLAN BUY UP PLAN ANNUAL DEDUCTIBLE EMPLOYEE AND EACH COVERED FAMILY MEMBER $50 per person, $50 per person, up to $150 per family up to $150 per family CALENDAR YEAR MAXIMUM (FOR COVERED SERVICES) EMPLOYEE AND EACH COVERED FAMILY MEMBER $1,000 per person $1,550 per person CLASS I: PREVENTIVE AND DIAGNOSTIC SERVICES COVERED AT* COVERED AT* ORAL EXAMS AND CLEANINGS (2X PER CALENDAR YEAR) X-RAYS: FULL MOUTH (1 EVERY 36 MONTHS) BITEWING (1 SERIES PER 12 MONTHS) 100%, no deductible 100%, no deductible FLUORIDE APPLICATION (1 PER CALENDAR YEAR; LIMITED TO DEPENDENT CHILDREN UNDER 16 YEARS OLD) SPACE MAINTAINERS (LIMITED TO NON-ORTHODONTIC TREATMENT) CLASS II: BASIC RESTORATIVE SERVICES FILLINGS, ENDODONTICS, PERIODONTAL SCALING, DENTURE ADJUSTMENTS AND REPAIRS, EXTRACTIONS, ANESTHETICS, ORAL SURGERY INCLUDING 50%** 80%** BONEY IMPACTED WISDOM TEETH CLASS III: MAJOR RESTORATIVE SERVICES CROWNS, DENTURES, BRIDGES 50%** 50%** 50%** CLASS IV: ORTHODONTIA LIFETIME MAXIMUM (FOR ORTHODONTIA SERVICES ONLY) No coverage APPLIES TO DEPENDENT CHILDREN LESS THAN 19 YEARS OF AGE $1,500 * Up to a maximum allowed charge (excludes exams, cleanings and x-rays) ** After plan deductible. Note Extraction of wisdom teeth, including bony impacted teeth, is covered under the Dental Plan only and requires pre-certi昀椀cation prior to services. 36
My Vision Bene昀椀ts UNUM Vision • www.alwaysassist.com • 866-679-3054 Vision Buy-Up Plan Vision health is an indicator of overall health. Regular eye exams can detect diseases like glaucoma, diabetes and loss of sight. Vision bene昀椀ts allow for access to quality vision care. To ensure that you and your family will get the care you need, FMOLHS now offers 2 comprehensive vision bene昀椀t plans provided by UNUM vision. Enrolled team members will also have access to hearing aid discounts. In-network copayments are paid directly to the provider. Out-of-network copayments will be deducted from the out-of-network reimbursement. » Contact lenses are in lieu of eyeglass lenses and frames bene昀椀t. » The insured is responsible for paying any charges in excess of this allowance. Network Providers offer the lowest out-of-pocket costs. To 昀椀nd a network provider, log on to www.alwaysassist.com and select provider locator. Eligibility Full-time and regular part-time (0.5 – 1.0 FTE) team members. Vision Premiums (semi-monthly; 24 deductions) VISION BASIC PLAN BUY UP PLAN 2023 PREMIUMS TEAM MEMBER $2.47 $3.05 TEAM MEMBER + SPOUSE $4.93 $6.11 TEAM MEMBER + CHILD(REN) $6.17 $7.64 TEAM MEMBER + FAMILY $6.79 $8.41 37
Vision Plan Summary BASIC PLAN BUY UP PLAN IN-NETWORK OUT-OF-NETWORK IN-NETWORK OUT-OF-NETWORK COPAY EXAMINATION $10 copay Up to $35 allowance $10 copay Up to $50 allowance MATERIALS $15 copay See covered services $10 copay See covered services BENEFIT FREQUENCY EXAMINATION 12 months 12 months 12 months 12 months LENSES 12 months 12 months 12 months 12 months FRAMES 12 months 12 months 12 months 12 months CONTACTS 12 months 12 months 12 months 12 months (in lieu of Lenses and Frames) COVERED MATERIALS STANDARD PLASTIC LENSES* SINGLE VISION LENSES 100% after copay Up to $25 allowance 100% after copay Up to $50 allowance BIFOCAL LENSES 100% after copay Up to $40 allowance 100% after copay Up to $60 allowance TRIFOCAL LENSES 100% after copay Up to $50 allowance 100% after copay Up to $70 allowance LENTICULAR $80 allowance Up to $50 $80 allowance Up to $70 allowance PROGRESSIVE $70 allowance Up to $40 $70 allowance Up to $60 allowance FRAMES 100% up to $100 allowance 100% up to $150 allowance RETAIL FRAME EQUIVALENT ($94 at Walmart, Sam’s Club Up to $50 allowance ($94 at Walmart, Up to $60 allowance and Costco) Sam’s Club and Costco) CONTACT LENSES 100% up to $100 allowance $100 up to $150 allowance ELECTIVE Up to $100 allowance $100 allowance (in lieu of frames) (in lieu of frames) MEDICALLY NECESSARY 100% after copay Up to $210 100% after copay Up to $210 *Scratch resistant coating and Polycarbonate Lenses for children are covered at Walmart only. Note Members receive a discount on LASIK or PRK prices with participating surgery providers. 38
My Health Savings Accounts – HSA Take charge of your health care spending with a Health Savings Account (HSA). Contributions to an HSA are tax free and withdrawals for quali昀椀ed medical expenses are tax free. Your HSA can be used for quali昀椀ed expenses, including those of your spouse and/or taxable dependent(s), even Individually Owned Account You own and administer your Health Savings Account. if they are not covered by your plan. If you are not You determine how much you’ll contribute to the account, enrolled in a HDHSA but you have unused HSA funds from a previous account, those funds can still be used when to use the money to pay for quali昀椀ed medical expenses, and when to reimburse yourself. HSAs allow for quali昀椀ed medical expenses. you to save and roll over money if you do not spend it in PayFlex will issue you a debit card, giving you direct the calendar year. The money in this account is portable, access to your account balance. When you have a even if you change plans or jobs. There are no vesting quali昀椀ed medical expense, you can use your debit card requirements or forfeiture provisions. to pay. You must have a balance to use your debit card. There are no receipts to submit for reimbursement. How to Enroll Eligible expenses include doctors’ of昀椀ce visits, eye You must elect the HDHSA plan with FMOLHS. You exams, prescription expenses, laser eye surgery and will need to complete all HSA enrollment materials and more. IRS Publication 502 provides a complete list of designate the amount to contribute on a pre-tax basis. eligible expenses and can be found on www.irs.gov. FMOLHS will establish an HSA account with PayFlex in your name and send in your contribution once bank account information has been provided and veri昀椀ed. Eligibility You are eligible to open and fund an HSA if: » You are enrolled in the HDHSA plan. Maximize Your Tax Savings » You are not covered by your spouse’s HDHSA plan. Contributions to an HSA are tax-free (they can be made » Your spouse does not have a Medical Flexible through payroll deduction on a pre-tax basis when you open an account with PayFlex). The money in this account Spending Account (FSA) or Health Reimbursement (including interest and investment earnings) grows Account (HRA). tax-free. As long as the funds are used to pay for quali昀椀ed » You are not eligible to be claimed as a dependent medical expenses, they are spent tax-free. on someone else’s tax return. Per IRS regulations, if HSA funds are used for purposes » You are not enrolled in Medicare or TRICARE. other than quali昀椀ed medical expenses and you are » You have not received Department of Veterans younger than age 65, you must pay federal income tax on the amount withdrawn, plus a 20% penalty tax. Affairs medical bene昀椀ts in the past 90 days for non-service-related care. (Service-related care will not be taken into consideration.) 39
HSA Funding Limits FMOLHS will provide an HSA employer contribution that will be deposited on an annual basis ONLY if the employee contributes to the HSA. Each year, the IRS places a limit on the maximum amount that can be contributed to HSA accounts. For 2023, contributions are limited to the following: TEAM MEMBER TOTAL EMPLOYER CONTRIBUTION CONTRIBUTION CONTRIBUTION MAXIMUM MAXIMUM TEAM MEMBER $3,100 $750 $3,850 FAMILY $6,250 $1,500 $7,750 CATCH-UP (AGES 55+) $1,000 N/A N/A Employee HSA contributions in excess of the IRS annual contribution limits ($3,100 for individual coverage and $6,250 for family coverage for 2023) are not tax deductible and are generally subject to a 6% excise tax. If you’ve contributed too much to your HSA this year, you can do one of two things: » Remove the excess contributions and the net income attributable to the excess contribution before you 昀椀le your federal income tax return (including extensions). You’ll pay income taxes on the excess removed from your HSA. » Leave the excess contributions in your HSA and pay 6% excise tax on excess contributions. Next year you may want to consider contributing less than the annual limit to you HSA to make up for the excess contribution during the previous year. The FMOLHS HSA will be established with PayFlex. You may be able to roll over funds from another HSA. For more enrollment information, contact PayFlex or visit www.pay昀氀ex.com. Note For more information on Health Savings Accounts (HSA) visit www.pay昀氀ex.com 40
My Flexible Spending Account – FSA PayFlex www.pay昀氀ex.com • 844-PayFlex (729-3539) FSA Debit Card: Medical Flexible FLEXIBLE SPENDING ACCOUNT (FSA) Spending Account MEDICAL FSA LIMITED USE FSA HOW MUCH CAN I The FSA Debit Card allows you to pay for eligible health $2,750 per year $2,750 per year CONTRIBUTE? care expenses at the point of service and deducts funds directly from your FSA account. Over-the-counter (OTC) WHO IS ELIGIBLE? 0.5 – 1.0 FTE 0.5 - 1.0 FTE purchases require a doctor’s prescription in order for the PayFlex will administer the Medical and Limited Use OTC medicine or drug to be eligible for reimbursement Flexible Spending Accounts. from an FSA. For OTC purchase reimbursement, you will have to substantiate the purchase by submitting your Medical Flexible Spending Account receipt and doctor’s prescription to PayFlex. You may use The Health Care FSA allows you to set aside money your FSA Debit Card at locations such as doctors’ and through payroll deductions on a pre-tax basis to pay for dentists’ of昀椀ces, pharmacies, and vision service providers. out-of-pocket health care expenses, such as deductibles, The card cannot be used at locations that do not offer copays, coinsurance, prescribed medications, dental services under the Plan, unless the provider has also expenses, vision expenses, Lasik and more. By paying complied with IRS regulations. Should you attempt to use for these expenses with pre-tax dollars, you reduce the card at an ineligible location the swipe transaction the amount of your taxable income and increase your will be denied. Should you need to submit a receipt, take-home pay. you will receive an email or mailed Receipt Noti昀椀cation from PayFlex, but you should always retain a receipt for your records. Limited Use Flexible Spending Account General FSA Rules and Restrictions Designed to complement a Health Savings Account, a In exchange for the tax advantages FSAs offer, the IRS Limited Use Flexible Spending Account (LUFSA) allows for has imposed the following rules and restrictions for reimbursement of eligible Dental and Vision expenses. Health Care FSAs: If you enroll in the HSA account and also enroll in the Medical FSA in 2023, the Medical FSA automatically » Your expenses must be incurred during the Plan becomes a Limited Use FSA (LUFSA). You must decide year of 2023. how much to set aside for this account. You may » Your dollars cannot be transferred from one FSA contribute up to $2,750 in the LUFSA. Again the LUFSA to another. can only be used for eligible dental and vision expenses. » You must “use it or lose it”— any unused funds will When you use your PayFlex debit card to pay for eligible be forfeited. dental and vision expenses, the available dollars will always pull from the LUFSA 昀椀rst until that account is » You cannot change FSA election in the middle of exhausted and then the dollars will pull from your the Plan year unless you have a quali昀椀ed life status HSA account. change, such as a marriage, divorce, or birth of Note a child. If you have any money remaining in your FSA at the end of the year, you forfeit it. In other words, "USE IT OR LOSE IT." 41
Please note: Itemized receipts/statements showing 2.5-Month Grace Period » The 2.5-month grace period allows participants an prior balances or ‘estimated’ insurance payments will not be acceptable. If insurance is indicated, the receipt/ additional period of time to incur expenses after the statement must show insurance payment posted and Plan year ends (December 31, 2023). 昀椀nal patient responsibility. Credit card receipts are » If an expense is incurred between January 1, 2023 and not acceptable forms because they do not provide the speci昀椀c item purchased; therefore, PayFlex cannot March 15, 2024 AND submitted for reimbursement on determine if the expense was an FSA eligible item. or before March 31, 2024, any remaining balance in the previous Plan year that ended December 31, 2023, will I thought purchases at certain vendors were be paid out for the claim, even though the service was automatically substantiated and considered provided in the NEW Plan year. approved purchases? As of February 2009, no additional substantiation is FSA FAQs required for debit card transactions that are approved at What should I do if I receive a substantiation letter or the point of sale by merchants (speci昀椀cally pharmacies) online noti昀椀cation? who have adopted the Inventory Information Approval System (IIAS). The IIAS system compares the SKU on Include these notices when you submit your receipts to the item being purchased to a list of FSA eligible items PayFlex. Keep a copy of these letters and copies of all sold at the store. When a FSA debit card is used, the receipts for your records. You can substantiate a claim by: pharmacy will only allow the card to pay for the FSA eligible items and any non-FSA eligible items will need MAIL FAX UPLOAD to be paid for using an alternative method of payment. If www.pay昀氀ex.com PayFlex Systems USA, Inc. 855-703-5305 Select Learn More merchants still have not adopted this system, FSA debit Flex Claims Department Use letter as your next to Substantiation P.O. Box 981158 cards might not work at their places of business. cover sheet Alert and click El Paso, TX 79998-1158 Upload My Receipts Contact Information: If I do not comply with these substantiation notices, You can reach Customer Service at: 844-729-3539 will I lose the ability to use my debit card? Send Claims To: PayFlex Systems USA, Inc. Yes, if you do not respond within the period of time noted Flex Department on the second noti昀椀cation, your card will be deactivated P.O. Box 981158 until acceptable documentation or payment is provided El Paso, TX 79998-1158 to PayFlex. How can I access my FSA dollars when my debit card is deactivated? You can purchase eligible items or services with another form of payment and submit a claim form along with receipts to PayFlex while your card is inactive. What are acceptable forms of substantiation? » An Explanation of Bene昀椀ts (EOB) is the preferred form of documentation. » An itemized receipt is also acceptable, but it must show: – Date of purchase or service – Amount of purchase or service – Description of item or service – Name of merchant or service provider – Name of patient if a medical claim 42
My Life Insurance Lincoln Financial Group www.LincolnFinancial.com/FMOLHS • 855-818-2883 Basic Life and Accidental Death and GROUP LIFE Dismemberment (AD&D) Insurance COVERAGE AMOUNT 1.5x annual salary Basic Life and Accidental Death and Dismemberment WHO PAYS Company pays full cost (AD&D) is a part of the FMOLHS bene昀椀ts plan and is WHEN BENEFITS ARE an essential part of your future 昀椀nancial security. It is PAYABLE If you die while covered under the plan important to understand how your plan works and what MAXIMUM BENEFIT $50,000 bene昀椀ts you will receive. Your Basic Life insurance bene昀椀t is equal to 1.5 times your WHEN CAN I CHANGE basic annual earnings up to a maximum of $50,000. This MY ELECTION N/A bene昀椀t is provided at no cost to you. If you are eligible (0.5 – 1.0 FTE) you are automatically enrolled in Basic Employee Basic Life and AD&D Insurance will be reduced Life insurance through Lincoln National Life Insurance as follows: Company. AGE REDUCTION Beneficiary Designation At age 65 Bene昀椀t will reduce by 35% of the original amount Your bene昀椀ciary designation is the person you name to At age 70 Bene昀椀t will reduce an additional 15% of the original amount receive your life insurance bene昀椀ts in the event of your At age 75 Bene昀椀t will reduce an additional 15% of the original amount death. This includes any life insurance bene昀椀ts payable At retirement Bene昀椀t will terminate when the insured person retires under the Supplemental or Voluntary Life insurance plans available through FMOLHS. Bene昀椀ts payable If a team member 昀椀rst enrolls for Employee Life and for a dependent’s death under the Dependent Life AD&D Insurance at age 65 or older, the above age insurance plan are payable to you if living; otherwise, if no reductions will apply to any guarantee issue amount and bene昀椀ciary is listed, the insurance company will specify to the maximum eligible amount. the bene昀椀ciary based on contract guidelines. The primary purpose of life insurance is to provide 昀椀nancial support to a bene昀椀ciary when he or she needs it most – at the loss of a loved one. Therefore, it is very important your bene昀椀ciary designations be kept up to date. Note It is important that you name a primary and contingent bene昀椀ciary to receive your Life Insurance bene昀椀ts. You can designate a bene昀椀ciary when making your New Hire/Newly Eligible bene昀椀t elections in Oracle Employee Self Service under Me/Bene昀椀ts. When making your elections, you will be prompted to designate a bene昀椀ciary under the Life Insurance section. 43
My Retirement Bene昀椀ts Our retirement bene昀椀ts are a cornerstone of our bene昀椀t program and demonstrate our support for you as you plan for your future. Our goal is to ensure we have a strong, sustainable bene昀椀t for many years to come while continuing to invest as we always have in our team members' future. We’re also recognizing the increasing desire for team members to have more control of their retirement bene昀椀ts and how they plan for their future. What’s included in this section (and why it’s important) » Snapshot of our retirement plans » How to enroll – Steps to enroll in the FMOLHS 403(b) plan during open enrollment » What to do and resources to help You will enroll and make contribution election changes to all of our retirement plans directly on our custom Lincoln Financial website at www.LincolnFinancial.com/FMOLHS. Snapshot of Our Retirement Plans The 403(b) retirement program allows you more control over how much you save, investment decisions and to select from a variety of fund options. As your retirement planning partner, FMOLHS is committed to providing you with a robust plan that is designed to help you pursue your retirement goals, and help you build even bigger dreams. With the retirement program, you will enjoy a host of bene昀椀ts, including: Employer matching contributions (see below for details) » Employer core » A range of diverse investment options retirement contributions » Exceptional website and customer » A fully portable plan that moves service support with you when you retire or » Ability to make hardship withdrawals change jobs or plan loans, if certain criteria are met » Greater control over » Ability to make withdrawals from investment decisions your account at age 59½, even if » A robust plan website accessible via you are actively employed computer, mobile or wearable app » Personalized expert help from on-site Lincoln Financial retirement consultants 44
My Retirement Bene昀椀ts 403(b) Savings Plan » Employer Contribution: If you work at least 1,000 hours and are employed on the last day of the year, you are eligible for a core contribution of 2% of your pay into your 403(b) account – FMOLHS will make a core contribution if you meet the requirements for hours worked and employment as of the last day of the calendar year even if you choose not to contribute your own money into the account. – Employer core contribution will be made annually » New Hires: You will be automatically enrolled at 4%. You may change your deferral rate or opt-out at any time. » You may elect to contribute anywhere from 1% to 100% directly from your paycheck, pre-tax or Roth after-tax; you are always 100% vested in your contributions Employer Match Contribution Account » You are eligible if you are contributing to the 403(b). » You must work at least 1,000 hours and be employed on the last day of the calendar year to be eligible. » FMOLHS will provide a 50% matching contribution for each dollar you contribute to the 403(b) plan, up to the 昀椀rst 6% (3% maximum). » Matching contributions will be made annually Vesting » FMOLHS employer and matching contributions are 100% vested after 3 years of service. Note You will enroll and manage your retirement accounts — 403(b) and 457(b) — directly on the Lincoln Financial website at LincolnFinancial.com/FMOLHS. 45
What to Do and Resources to Help HOW TO ENROLL » Register and secure your account at LincolnFinancial.com/Register. REGISTER » Log into your account at LincolnFinancial.com/Retirement. You must take action to enroll. » Select the amount you’d like to contribute, » Con昀椀rm your investment option — either the default investment or one you prefer — ENROLL – and click Submit. That’s it! You’re enrolled. – You may also elect to set up an automatic contribution increase » Make sure you designate your bene昀椀ciary for each retirement account BENEFICIARY AND E-DELIVERY » Sign up for E-Delivery to receive your quarterly statement RESOURCES TO HELP YOU » Detailed information about all of the retirement plans is available on our Total Rewards page and www.LincolnFinancial.com/FMOLHS. » If you have questions about your retirement plan, Contact: call the Lincoln Customer Contact Center at Ryan Jones 877-562-4738 and speak to a Customer [email protected] 403(b) SAVINGS PLAN (EMPLOYER 225-305-8539 CONTRIBUTION AND MATCH), 457(b) PLAN Service Representative weekdays from 9:00 a.m. Jayme Schwartzenburg to 7:00 p.m. Central. [email protected] » To receive personal assistance, go to 225-363-8767 LincolnFinancial.com/FMOLHSschedule to schedule a free one-on-one personal consultation or contact one of your Lincoln Financial retirement consultants. ® Lincoln WellnessPATH Your Path to Financial Wellness Wellness isn’t just about physical health. There are emotional and 昀椀nancial components, too. Whether you want to save more or need to pay off debt, getting your 昀椀nances in order can have an impact on your overall well-being. It can help you move forward with con昀椀dence and be ready for whatever life brings. That’s where Lincoln can help. ® Lincoln WellnessPATH provides tools and personalized steps to manage your 昀椀nancial life. From creating a budget to building an emergency fund to paying down debt, our easy-to-use online tool helps you turn information into action so you can focus on both short- and long-term goals, such as saving for retirement. To get started, log in to your account at LincolnFinancial.com/WellnessPATH. 46
My Disability Insurance Short Term Disability Insurance » Eligible Members (0.5 – 1.0 FTE); Coverage is effective on the 91st day of continuous eligibility. » Employer-paid – no cost to team members. » Short Term Disability (STD) insurance protects a portion of your income if you become partially or totally disabled for a short period of time. GROUP SHORT TERM DISABILITY COVERAGE AMOUNT Up to 60% of basic annual Earnings WHO PAYS Company pays full cost WHEN BENEFITS ARE PAYABLE Following 7 days of illness or injury MAXIMUM BENEFIT DURATION 12 weeks Certain exclusions apply. Please refer to My Bene昀椀ts on our Total Rewards page at fmolhs.org/totalrewards. Long Term Disability Insurance Lincoln Financial Group • LincolnFinancial.com/FMOLHS • 855-818-2883 LONG TERM DISABILITY GROUP CORE LTD GROUP BUY-UP LTD COVERAGE AMOUNT 50% of basic monthly salary 60% of basic monthly salary WHO PAYS Employee & company share cost Employee pays full cost WHEN BENEFITS ARE PAYABLE Following 90 days of disability Following 90 days of disability MAXIMUM MONTHLY BENEFIT $3,000 per month $10,000 per month WHEN EVIDENCE OF INSURABILITY IS REQUIRED Any election after original enrollment period Any election after original enrollment period » Eligible Members (0.8 – 1.0 FTE) » You must participate in the Core Plan to be eligible for the Buy-up option Long Term Disability (LTD) insurance protects a portion of your income if you become partially or totally disabled for a long period of time. You must be disabled for at least 90 days before you can receive a Long Term Disability insurance bene昀椀t payment. Payments will last for as long as you are disabled or until you reach your Social Security Normal Retirement Age, whichever is sooner. If you may be entitled to some other income bene昀椀t, you are required to actively pursue it. Any other bene昀椀ts you receive (such as Social Security Disability, Workers’ Compensation, pension bene昀椀ts or bene昀椀ts from any similar act or plan) will reduce your LTD bene昀椀ts. Certain exclusions, as well as pre-existing condition limitations, may apply. Please refer to My Bene昀椀ts on our Total Rewards website at fmolhs.org/totalrewards. 47
My Voluntary Bene昀椀ts FMOLHS offers special voluntary bene昀椀ts, through Lincoln Life Insurance Company to all eligible team members. These bene昀椀ts are designed to provide 昀椀nancial security at an affordable price. VOLUNTARY BENEFIT PLANS PLAN NEW ENROLLEES FUTURE ENROLLEES Team members who are within their 昀椀rst 30 days of Enrollment in coverage is not available LINCOLN VOLUNTARY EMPLOYEE LIFE eligibility may enroll through Oracle Employee Self at any future date for team members Service. Team Members may elect coverage in $10,000 who do not enroll within their 昀椀rst increments up to a maximum of $150,000. 30 calendar days of eligibility. LINCOLN VOLUNTARY SPOUSE LIFE Team members who are within their 昀椀rst Enrollment in coverage is not available at any future LINCOLN VOLUNTARY DEPENDENT LIFE 30 days of eligibility may enroll through date for team members who do not enroll within their Oracle Employee Self Service. 昀椀rst 30 calendar days of eligibility. Team members who are within their 昀椀rst Eligible to enroll in coverage during LINCOLN VOLUNTARY ACCIDENT 30 days of eligibility may enroll through annual Open Enrollment period. Oracle Employee Self Service. Team members who are within their 昀椀rst Eligible to enroll in coverage during LINCOLN VOLUNTARY CRITICAL ILLNESS 30 days of eligibility may enroll through annual Open Enrollment period. Oracle Employee Self Service. These policies are portable. If coverage under these policies ends for any reason other than non-payment of premium or your spouse or dependent child ceasing to meet the de昀椀nition of an eligible dependent, they are eligible for portability. To port your coverage, contact Lincoln Financial Group within 31 days of your coverage terminating and pay the applicable premium. (See your certi昀椀cate for details.) Eligible dependents for these plans include your legal spouse and dependent children as de昀椀ned below by bene昀椀t. » Voluntary Life Bene昀椀ts – Unmarried dependent children to age 21; to age 25 if a full time student. » Voluntary Accident and Critical Illness Bene昀椀ts – To age 26 regardless of marital status or student status. Note: Please ensure that you are managing your dependent child’s eligibility and enrollment in these plans. Eligibility is only reviewed by Lincoln at the time of a claim. Voluntary Critical Illness Critical Illness coverage can help and it's affordable. If a serious illness strikes, the last thing you want to worry about is bills. With Critical Illness insurance, you can get a cash bene昀椀t even if you’re receiving bene昀椀ts from other insurance. Use the cash for anything you want or need. SM Lincoln CareCompass services: your guide to being well even if you’re sick. Of course, money isn’t everything, SM especially when someone is critically ill. That’s why our Critical Illness coverage comes with Lincoln CareCompass bene昀椀ts and services to help you before, during and after a critical illness. » You do not have to be terminally ill to receive bene昀椀ts. » Coverage is available for you and your spouse. Eligible children are covered for $5,000 at no additional cost. » A Health Screening Bene昀椀t is included, which provides a $75 bene昀椀t per insured team member and/or spouse per calendar year for a covered health screening test. » Coverage is portable — you can take your plan with you if you change jobs or retire. (See your certi昀椀cate for details.) 48
Please note that these are just highlights of the enhanced bene昀椀ts being offered to you and limitations and exclusions apply. Please contact Lincoln for a complete list of limitations and exclusions. VOLUNTARY CRITICAL ILLNESS INSURANCE POLICY HIGHLIGHTS BENEFIT OPTIONS BENEFIT DETAIL EMPLOYEE $10,000 or $20,000 SUPPLEMENTAL BENEFITS SPOUSE $10,000 ADVANCED ALZHEIMER'S 100% CHILD EMBEDDED 25% ADVANCED PARKINSON'S 100% GUARANTEE ISSUE ADVANCED ALS 100% 100% – after 12 month treatment RECURRENCE (SAME CONDITIONS) ADVANCED MS 25% free ADVANCED COPD 100% MAXIMUM COVERED CONDITIONS Unlimited LOSS OF SPEECH 25% PRE-EXISTING 12/12 LOSS OF SIGHT 25% BENEFIT WAITING PERIOD None LOSS OF HEARING 25% AGE REDUCTIONS None ACCIDENTAL INJURY BENEFIT DETAIL TRAUMATIC BRAIN INJURY 100% CORE BENEFITS SEVERE BURNS 100% HEART ATTACK 100% PERMANENT PARALYSIS 100% ARTERIAL / VASCULAR DISEASE 25% CHILD CONDITIONS STROKE 100% SPINA BIFIDA 100% INVASIVE CANCER 100% CYSTIC FIBROSIS 100% NON-INVASIVE CANCER 25% MUSCULAR DYSTROPHY 100% SKIN CANCER $250 CEREBRAL PALSY 100% MAJOR ORGAN FAILURE 100% TYPE 1 DIABETES 100% RENAL (KIDNEY) FAILURE 100% CLEFT LIFE/PALATE 100% OCCUPATIONAL DISEASE DOWN'S SYNDROME 100% OCCUPATIONAL HIV 100% HEALTH ASSESSMENT BENEFIT OCCUPATIONAL HEPATITIS 100% $75 TUBERCULOSIS 25% MRSA 25% 49
Voluntary Accident We provide cash for accidental injuries, and you decide the best way to spend it. And because your employer offers this coverage at a group rate, it’s protection you can afford. Accident Insurance » Pays cash for accidental injuries » Includes travel assistance » Covers multiple injuries from the same accident » Includes on the job accidents » Is available for spouses and children » Is available at an affordable rate VOLUNTARY ACCIDENT INSURANCE POLICY HIGHLIGHTS BENEFITS BENEFITS EMERGENCY CARE RECOVERY BENEFITS AMBULANCE $225 FAMILY CARE $50 INITIAL CARE $75 COMPANION LODGING $100 EMERGENCY CARE TREATMENT $150 TRANSPORTATION $200 FRACTURE BENEFIT (NON-SURGICAL) CHILD SPORTS INJURY BENEFITS PER FRACTURE $100 -– $3,500 CHILD INJURY Additional 25% SURGICAL TREATMENT 2x non-surgical bene昀椀t ACCIDENTAL DEATH & DISMEMBERMENT CHIP FRACTURES 25% TEAM MEMBER $25,000 SPOUSE $10,000 DISLOCATION BENEFITS (NON-SURGICAL) PER INJURY $100 – $2,625 CHILD $5,000 SURGICAL TREATMENT 2x non-surgical bene昀椀t TRANSPORTATION OF REMAINS $5,000 LOSS OF OR LOSS OF USE OF: HAND, PARTIAL DISLOCATION 25% FOOT, ARM, LEG, EYE, HEARING $5,000 – $10,000 SPECIFIC INJURY BENEFITS MOTOR VEHICLE BENEFITS BLOOD TRANSFUSION $375 MOTOR VEHICLE INJURY $100 BURNS, 2ND OR 3RD DEGREE $100 – 10,000 MOTOR VEHICLE DEATH $2,500 SEVERE TRAUMATIC BRAIN INJURY $5,000 SEATBELT Additional 25% of motor vehicle injury or death bene昀椀t CONCUSSION $150 AIRBAG Additional 25% of motor vehicle DENTAL CROWN $150 injury or death bene昀椀t DENTAL EXTRACT $75 HELMET Additional 25% of motor vehicle injury or death bene昀椀t EYE (REMOVAL OF FOREIGN BODY) $150 SAFE RIDER (BICYCLE, SCOOTER, EYE (SURGICAL REPAIR) $300 SKATEBOARD, ETC.) $100 LACERATION $35-400 HELMET $100 HEALTH ASSESSMENT BENEFIT SURGICAL BENEFITS COVERED BENEFITS: PER SURGERY $150 – $1,500 REPAIR OF LIGAMENTS, TENDONS, Dental Preventive Exams, Annual Physical, Eye Exam, Hearing Exam, ROTATOR CUFF, KNEE CARTILAGE, $750 RUPTURED DISC Depression Screening, Substance Abuse Screening/Counseling, and Tetanus Immunization, Additional Adult Tests: HOSPITAL & ONGOING CARE BENEFITS $50 Osteoporosis Screening (Bone Mineral HOSPITAL ADMISSION $1,000 Density). Accident/Fall prevention HOSPITAL CONFINEMENT $200 counseling. Additional Child Tests: Sports/School Physicals, Concussion PHYSICIAN FOLLOW-UP $75 Screening, Immunizations (DTP, MMR, ALTERNATE CARE AND Rotavirus, Chickenpox, Meningitis) REHABILITATIVE CONFINEMENT $150 OCCUPATIONAL, PHYSICAL, SEMI-MONTHLY (24 DEDUCTIONS) CHIROPRACTIC THERAPY $35 TEAM MEMBER ONLY $3.96 PAIN MANAGEMENT $75 TEAM MEMBER + SPOUSE $5.77 MEDICAL MOBILITY DEVICES (CANE, KNEE WALKER, WALKER, CRUTCHES, $75 TEAM MEMBER + CHILD(REN) $6.97 WALKING BOOT) TEAM MEMBER + FAMILY $9.24 WHEELCHAIR $150/$300 PROSTHESIS $750 50
Voluntary Term Life Insurance Live for now. Plan for then. Every day, you provide for the ones you love. You make sure they’re happy and secure, with thoughtful touches to let them know you care. Life insurance lets you plan for the future and continue to show your love even after you’re gone. Life insurance can help: » Protect your loved ones from 昀椀nancial burdens » Pay for your children’s or grandchildren’s education » Build a secure retirement fund for your spouse or partner » Assist a disabled adult child » Leave a legacy for your loved ones or a favorite charity Policy Highlights Eligibility (for Team Members and Dependents): All Active full time and part time team members 0.5 – 1.0 FTE. A delayed effective date will apply if the team member is not actively at work. Spouse and dependents cannot be in a period of limited activity on the day coverage takes effect. Unmarried Dependent Child(ren) are eligible from age 14 days to age 21; age 25 if a full time student. VOLUNTARY VOLUNTARY VOLUNTARY EMPLOYEE LIFE SPOUSE LIFE DEPENDENT LIFE Team members who are within their 昀椀rst 30 days of eligibility may enroll through Team members who are within their 昀椀rst Oracle Employee Self-Service. Team members who are within their 昀椀rst 30 days of eligibility may enroll through 30 days of eligibility may enroll through Oracle Employee Self-Service. You must be enrolled in Oracle Employee Self-Service. Voluntary Employee Life in order WHEN YOU CAN ENROLL Team members may enroll in $10,000 to elect Spouse coverage. You must be enrolled in Voluntary increments up to a maximum of Employee Life in order to elect $150,000. Spouse coverage amount Dependent coverage. cannot exceed the employee’s elected If you terminate coverage, you will not coverage amount. If you terminate coverage, you will not have an opportunity to re-enroll. have an opportunity to re-enroll. If you terminate coverage, you will not have an opportunity to re-enroll. COVERAGE AMOUNT $10,000 increments $10,000 increments $10,000 MAXIMUM BENEFIT $150,000 initial enrollment $30,000 $10,000 Coverage is portable — you can take your coverage with you if you leave the company. To port your coverage, contact Lincoln Financial Group within 31 days of your coverage terminating and pay the applicable premium. (See your certi昀椀cate for details.) Note You can designate a bene昀椀ciary when making your New Hire/Newly Eligible bene昀椀t elections in Oracle Employee Self Service under Me/Bene昀椀ts. When making your elections, you will be prompted to designate a bene昀椀ciary under the Life Insurance section. 51
My EAP New Directions www.ndbh.com • 800-624-5544 When life’s a little much, reach out and get in touch. Let’s be real: life can be tough. When your responsibilities start to feel overwhelming and showing up each day with a smile on your face seems dif昀椀cult, it’s important to reach out for help. You can lean on your free and con昀椀dential Employee Assistance Program (EAP) for support. We’ve got your back. A free bene昀椀t from your workplace, the EAP can help you or anyone in your household: » Be more present and productive at work » Receive support when you don’t feel like yourself » Get help with responsibilities that are distracting or stressful » Grow personal and career skills » Be a caring, loving friend or family member » Receive care after a traumatic event or diagnosis » Make healthy lifestyle choices » Improve and inspire daily life We’re here for you, always. Life happens, regardless of the day or time. That’s why we make ourselves available 24/7, even on holidays. So whenever you need to reach out, we’re here for you. 52
53
My Discounts Team members may register on the Access Perks site and enter their personal email to receive emails with updates about available discounts or access discounts through the App or website. The company sponsors this bene昀椀t for the employees and there are no premiums or elections required to participate. What is Access Perks? Access Perks is a team member discount program that includes both Local and National group discounts » All employed team members are eligible to participate (FMOLHS will provide Access Perks with a demographic 昀椀le that includes an employee number that will identify your eligibility) » Your employee ID will be the 昀椀rst two letters of your 昀椀rst name and your Oracle ID (ex. ABXXXXX) » Members will have access to discounts through the Access Perks Web Portal or the My Deals Mobile App » Mobile App has a GPS/Geolocation functionality that allows users to 昀椀nd deals nearby instantly no matter if they are close to home or traveling Contact Access Perks at 877-408-2603 or visit the website at FMOLHS.AccessPerks.com. How do I Access the Mobile App? Accessing the mobile app is easy, all you need to do is go into the Apple Store or GooglePlay and search for “Access Perks.” Once you have downloaded the app, you will be able to open it and register by clicking “Set Up Account.” Once your registration is complete and you have set your password you are ready to start saving at thousands of participating providers. Some great examples are listed below: 54
Franciscan Missionaries of Our Lady University (FranU) Discounts Mission Statement: The mission of Franciscan Missionaries of Our Lady University is to educate and form Franciscan servant leaders of all faiths. We honor and preserve the legacy of our founders by preparing highly skilled professionals, integrated thinkers, and faith-昀椀lled citizens. Inspired by the Franciscan Missionaries of Our Lady to be a living witness to Jesus Christ and the Gospel message, the University is in communion with the teachings of the Catholic Church. Non-University FMOLHS Employee Discounts We offer discounts to help our Health System Heroes get the education that they deserve. FMOLHS invests back into the people who invest their time in our organization. We offer a 50% employee discount and a 40% dependent of an employee discount on the following programs: Undergraduate Programs Associate Degree Bachelor of Arts » Physical Therapist Assistant » Theology » Radiological Technology » Psychology Bachelor of Science Bachelor of Business Administration » Health Sciences » Business Administration – Biology track – General Business track – Health Service Administration track – Health Administration track – Psychology track – Management track » Medical Laboratory Science – MLS – MLT-MLS » Nursing – Pre-Licensure Nursing (BSN) – Online RN-BSN Note » Respiratory Therapy For more information on the programs, » Biology reach out to FranU: – Biochemical Analysis & Instrumentation Call: 225-526-1631 (BAI) track – Pre-Professional Human Medicine track Email: [email protected] – Accelerated 3 + 2 Pathway to Physician Assistant Studies 55
Helping You Balance Your Work and Personal Life Studies show that team members who are healthy and happy are those who have achieved a good balance between their work and personal responsibilities. To help you achieve this balance, the Health System offers numerous bene昀椀ts that allow you to spend more time with your friends and family, recover from an illness, enjoy your holidays or pursue other interests. Each of these bene昀椀ts are summarized in the table below. WHEN YOU ARE ELIGIBLE WHAT YOU RECEIVE BENEFITS Annual Accrual 0 – 4 years 132 hrs (16.5 days) 5 – 9 years 156 hrs (19.5 days) Immediately. 10 – 14 years 180 hrs (22.5 days) PAID TIME OFF (PTO) Eligible full time (AF) and part time (PT) 0.5 – 1.0 FTE 15 – 19 years 204 hrs (25.5 days) 20 – 24 years 228 hrs (28.5 days) Time may be used upon accrual 25 years + 252 hrs (31.5 days) PTO may be carried over to a max of 328 hours; part time PTO accrual rates are prorated (Years of service credit is determined by adjusted hire date) To assist with managing PTO accrual balances, team members PTO SELL BACK Eligible full time (AF) and part time (PT) 0.5 – 1.0 FTE may elect to “sell back” future PTO accruals. The combination Annually during the sell back period of PTO accruals and PTO sell back accruals will not exceed 328 hours. Hours in excess of 328 will not be paid out. Team members may receive a bi-weekly disability income bene昀椀t if they become disabled as a result of an injury or illness, including a pregnancy-related condition, while covered under Active full time (AF) and part time (PT) 0.5 to 1.0 FTE the short term disability. SHORT TERM DISABILITY Eligible Team members are automatically enrolled in the Short Term Disability bene昀椀t on the 91st day Important PAY information while on a leave of absence: of continuous eligibility. If you are on a leave of absence for your own illness and are eligible for short term disability, you must return all required leave documents to Leave Administration by the due date in order to initiate your disability claim. New Year’s Day, Good Friday, Independence Day, Labor Day, HOLIDAYS Immediately Thanksgiving Day and Christmas Day Active full time (AF) and part time (PT) 0.5 – 1.0 FTE Part time holiday accrual rates are prorated. Up to 3 scheduled work days (not to exceed 24 hours) paid leave for death in team member’s immediate family, BEREAVEMENT LEAVE Immediately de昀椀ned as parent, step-parent, brother, sister, spouse, Active full time (AF) and part time (PT) 0.5 – 1.0 FTE dependents (including stepchildren), parent-in-law (mother-in-law, father-in-law), grandchildren, grandparent, and great grandparent Immediately Time off from regularly scheduled work to serve on a JURY DUTY local, state or federal jury in response to a jury summons, All employed team members and may be eligible for jury compensation CONTINUING EDUCATION Immediately As approved Visit FMOLHS Total Rewards page under My Growth and EDUCATION ASSISTANCE See FMOLHS policy on TeamLink Development for more information. Free annual in昀氀uenza inoculation EMPLOYEE HEALTH SERVICES Immediately and Hepatitis B vaccine program Regular share savings account by direct deposit, signature CREDIT UNION Immediately loans, and new and used car loans Peer-based recognition of employees who exemplify core FRANCISCAN SERVICE AWARD Upon nomination values of the organization Up to 12 weeks leave for certain family and medical events. FAMILY & MEDICAL LEAVE (FMLA) After 1 year employed & 1,250 hours of service Apply for all Leave status online or contact Leave Administration: 833-4uaskHR (833-482-7547) 56
WHEN YOU ARE ELIGIBLE WHAT YOU RECEIVE BENEFITS PERSONAL LEAVE After 6 months Up to 4 weeks may be granted upon manager approval MEDICAL LEAVE Upon date of hire Up to 12 weeks Leave while serving in the “Uniformed Services” including MILITARY LEAVE Immediately voluntary and involuntary service and time spent in active duty, inactive duty training, and full time National Guard duty Employee and family blood bank program. Immediately EMPLOYEE’S BLOOD DONOR PLAN Participate by giving one unit of blood each year. HEALTH CENTER MEMBERSHIP Immediately Discounts on various memberships Medical expenses and wage replacement for on-the-job Immediately WORKERS’ COMPENSATION injuries/exposures as governed by state law Allows you to save money and earn rewards just for being a team member of FMOLHS. Team Members are automatically ACCESS PERKS Immediately enrolled at no cost and are eligible to receive discounts on purchases from thousands of local and national merchants Financial wellness app that gives you access to 40% of your PAY ACTIV Immediately earned but unpaid wages before your actual payday Team Members receive a 50% tuition discount for FRANU TUITION DISCOUNT See FranU policy on TeamLink undergraduate programs and their dependents receive a 40% tuition discount for undergraduate programs 57
Required Notices Required Notices When Will You Pay A Higher Premium (Penalty) To Join A Medicare Drug Plan? Important Notice from Franciscan Missionaries of You should also know that if you drop or lose your current coverage with Our Lady Health System About Your Prescription Drug Franciscan Missionaries of Our Lady Health System and don’t join a Medicare drug plan within 63 continuous days after your current coverage ends, you may Coverage and Medicare under the FMOLHS Health pay a higher premium (a penalty) to join a Medicare drug plan later. Plan(s) If you go 63 continuous days or longer without creditable prescription drug Please read this notice carefully and keep it where you can find it. This coverage, your monthly premium may go up by at least 1% of the Medicare notice has information about your current prescription drug coverage with base beneficiary premium per month for every month that you did not have that Franciscan Missionaries of Our Lady Health System and about your options under coverage. For example, if you go nineteen months without creditable coverage, Medicare’s prescription drug coverage. You are responsible for providing this your premium may consistently be at least 19% higher than the Medicare base notice to any Medicare eligible dependents covered under the Health Plan. This beneficiary premium. You may have to pay this higher premium (a penalty) as long information can help you decide whether or not you want to join a Medicare drug as you have Medicare prescription drug coverage. In addition, you may have to plan. If you are considering joining, you should compare your current coverage, wait until the following October to join. including which drugs are covered at what cost, with the coverage and costs of the plans offering Medicare prescription drug coverage in your area. Information For More Information about This Notice or Your Current about where you can get help to make decisions about your prescription drug Prescription Drug Coverage… coverage is at the end of this notice. Contact the person listed at the end of these notices for further information. There are two important things you need to know about your current coverage NOTE: You’ll get this notice each year. You will also get it before the next and Medicare’s prescription drug coverage: period you can join a Medicare drug plan, and if this coverage through 1. Medicare prescription drug coverage became available in 2006 to Franciscan Missionaries of Our Lady Health System changes. You also may request a copy of this notice at any time. everyone with Medicare. You can get this coverage if you join a Medicare Prescription Drug Plan or join a Medicare Advantage Plan (like an HMO For More Information about Your Options under or PPO) that offers prescription drug coverage. All Medicare drug plans provide at least a standard level of coverage set by Medicare. Some Medicare Prescription Drug Coverage… plans may also offer more coverage for a higher monthly premium. More detailed information about Medicare plans that offer prescription drug 2. Franciscan Missionaries of Our Lady Health System has determined that coverage is in the “Medicare & You” handbook. You’ll get a copy of the handbook in the prescription drug coverage offered by the FMOLHS Health plan(s) the mail every year from Medicare. You may also be contacted directly by Medicare is, on average for all plan participants, expected to pay out as much as drug plans. standard Medicare prescription drug coverage pays and is therefore For more information about Medicare prescription drug coverage: considered Creditable Coverage. Because your existing coverage is Creditable Coverage, you can keep this coverage and not pay a higher » Visit www.medicare.gov premium (a penalty) if you later decide to join a Medicare drug plan. » Call your State Health Insurance Assistance Program (see the inside back cover of your copy of the “Medicare & You” handbook for their telephone number) for personalized help WhenCanYouJoinAMedicare DrugPlan? » Call 1‑800‑MEDICARE (1‑800‑633‑4227). You can join a Medicare drug plan when you first become eligible for Medicare TTY users should call 1‑877‑486‑2048 during a seven‑month initial enrollment period. That period begins three months If you have limited income and resources, extra help paying for Medicare prior to your 65th birthday, includes the month you turn 65, and continues for the prescription drug coverage is available. For information about this extra help, ensuing three months. You may also enroll each year from October 15th through visit Social Security on the web at www.socialsecurity.gov, or call them at December 7th. 1‑800‑772‑1213 (TTY 1‑800‑325‑0778). However, if you lose your current creditable prescription drug coverage, through no fault of your own, you will also be eligible for a two (2) month Special Remember: Keep this Medicare Part D notice. If you decide to join one Enrollment Period (SEP) to join a Medicare drug plan. of the Medicare drug plans, you may be required to provide a copy of this notice when you join to show whether or not you have maintained What Happens To Your Current Coverage If You Decide to creditable coverage and, therefore, whether or not you are required to Join A Medicare Drug Plan? pay a higher premium (a penalty). If you decide to join a Medicare drug plan, your current Franciscan Missionaries of Our Lady Health System coverage will not be Date: January 1, 2023 affected. For most persons covered under the Plan, the Plan will pay prescription Name of Entity/Sender: Franciscan Missionaries of Our Lady Health drug benefits first, and Medicare will determine its payments second. For more System information about this issue of what program pays first and what program pays Contact—Position/Office: Human Resources second, see the Plan’s summary plan description or contact Medicare at the Address: PO Box 83780 telephone number or web address listed herein. Baton Rouge, LA 70884‑3780 If you do decide to join a Medicare drug plan and drop your current Phone Number: 833‑482‑7547 Franciscan Missionaries of Our Lady Health System coverage, be aware that you and your dependents will not be able to get this coverage back. 58 58
Women’s Health and Cancer Rights Act HIPAA Special Enrollment Rights If you have had or are going to have a mastectomy, you may be entitled to If you are declining enrollment for yourself or your dependents (including your certain benefits under the Women’s Health and Cancer Rights Act of 1998 spouse) because of other health insurance or group health plan coverage, you (WHCRA). For individuals receiving mastectomy‑related benefits, coverage will may be able to later enroll yourself and your dependents in this plan if you or be provided in a manner determined in consultation with the attending physician your dependents lose eligibility for that other coverage (or if the employer stops and the patient, for: contributing towards your or your dependents’ other coverage). » All stages of reconstruction of the breast on which the mastectomy Loss of eligibility includes but is not limited to: was performed; » Surgery and reconstruction of the other breast to produce a » Loss of eligibility for coverage as a result of ceasing to meet the plan’s symmetrical appearance; eligibility requirements (i.e. legal separation, divorce, cessation of » Prostheses; and dependent status, death of an employee, termination of employment, » Treatment of physical complications of the mastectomy, reduction in the number of hours of employment); including lymphedema. Loss of HMO coverage because the person no longer resides or works in » These benefits will be provided subject to the same deductibles and coinsurance the HMO service area and no other coverage option is available through applicable to other medical and surgical benefits provided under this plan. the HMO plan sponsor; For deductibles and coinsurance information applicable to the plan in which » Elimination of the coverage option a person was enrolled in, and another you enroll, please refer to the summary plan description. If you would like option is not offered in its place; Failing to return from an FMLA leave of absence; and more information on WHCRA benefits, please contact Human Resources at » 833‑482‑7547. » Loss of coverage under Medicaid or the Children’s Health Insurance Program (CHIP). HIPAA Privacy and Security Unless the event giving rise to your special enrollment right is a loss of coverage under Medicaid or CHIP, you must request enrollment within 30 days after your The Health Insurance Portability and Accountability Act of 1996 deals with how or your dependent’s(s’) other coverage ends (or after the employer that sponsors an employer can enforce eligibility and enrollment for health care benefits, as well as ensuring that protected health information which identifies you is kept that coverage stops contributing toward the coverage). private. You have the right to inspect and copy protected health information If the event giving rise to your special enrollment right is a loss of coverage that is maintained by and for the plan for enrollment, payment, claims and under Medicaid or the CHIP, you may request enrollment under this plan within case management. If you feel that protected health information about you is 60 days of the date you or your dependent(s) lose such coverage under Medicaid incorrect or incomplete, you may ask your benefits administrator to amend the information. For a full copy of the Notice of Privacy Practices, describing how or CHIP. Similarly, if you or your dependent(s) become eligible for a state‑granted protected health information about you may be used and disclosed and how you premium subsidy towards this plan, you may request enrollment under this can get access to the information, contact Human Resources at 833‑482‑7547. plan within 60 days after the date Medicaid or CHIP determine that you or the dependent(s) qualify for the subsidy. In addition, if you have a new dependent as a result of marriage, birth, adoption, or placement for adoption, you may be able to enroll yourself and your dependents. However, you must request enrollment within 30 days after the marriage, birth, adoption, or placement for adoption. To request special enrollment or obtain more information, contact ‑482‑7547. Human Resources at 833 59 59
NO SURPRISES ACT NOTICE Professional services rendered by independent healthcare professionals are not YOUR RIGHTS AND PROTECTIONS AGAINST SURPRISE MEDICAL BILLS part of the hospital bill. These services will be billed to the patient separately. Please understand that physicians or other healthcare professionals may be called upon to provide care or services to you or on your behalf, but you may When you get emergency care or get treated by an out‑of‑network not actually see, or be examined by, all physicians or healthcare professionals provider at an in‑network hospital or ambulatory surgical center, you are participating in your care; for example, you may not see physicians providing protected from surprise billing or balance billing. radiology, pathology, and EKG interpretation. In many instances, there will be a separate charge for professional services rendered by physicians to you or on your behalf, and you will receive a bill for these professional services that 1. What is “balance billing” (sometimes called “surprise billing”)? is separate from the bill for hospital services. These independent healthcare When you see a doctor or other health care provider, you may owe certain out‑ professionals may not participate in your health plan and you may be responsible of‑pocket costs, such as a copayment, coinsurance, and/or a deductible. You for payment of all or part of the fees for the services provided by these may have other costs or have to pay the entire bill if you see a provider or visit physicians who have provided out‑of‑network services, in addition to applicable a health care facility that isn’t in your health plan’s network. amounts due for copayments, coinsurance, deductibles, and non‑covered services. “Out‑of‑network” describes providers and facilities that haven’t signed a We encourage you to determine if independent healthcare professionals contract with your health plan. Out‑of‑network providers may be permitted to are participating in the Plan by checking the Plan’s website at www. bill you for the difference between what your plan agreed to pay and the full MyHealthToolkitLA.com/links/FMOLHS and/or calling Member Services at (833) amount charged for a service. This is called “balance billing.” This amount is 468‑3594. You may access these websites from home. If you have any questions likely more than in‑network costs for the same service and might not count about how to do this, please contact [email protected] or call 1‑833‑482‑7547. toward your annual out‑of‑pocket limit. “Surprise billing” is an unexpected balance bill. This can happen when you When balance billing isn’t allowed, you also have the following protections: can’t control who is involved in your care — like when you have an emergency » You are only responsible for paying your share of the cost (like the or when you schedule a visit at an in‑network facility but are unexpectedly copayments, coinsurance, and deductibles that you would pay if the treated by an out‑of‑network provider. provider or facility was in‑network). Your health plan will pay out‑of‑ network providers and facilities directly. 2. You are protected from balance billing for: » Your health plan generally must: » Cover emergency services without requiring you to get approval for Emergency services services in advance (prior authorization). If you have an emergency medical condition and get emergency services from – Cover emergency services by out‑of‑network providers. an out‑of‑network provider or facility, the most the provider or facility may bill – Base what you owe the provider or facility (cost‑sharing) on what it you is your plan’s in‑network cost‑sharing amount (such as copayments and would pay an in‑network provider or facility and show that amount in coinsurance). You can’t be balance billed for these emergency services. This your explanation of bene昀椀ts. includes services you may get after you’re in stable condition, unless you give – Count any amount you pay for emergency services or out‑of‑network written consent and give up your protections not to be balanced billed for these services toward your deductible and out‑of‑pocket limit. post‑stabilization services. If you believe you’ve been wrongly billed, you may contact the Department of Health care services may be provided to you at a network health care facility Health and Human Services (HHS) at 1‑800‑985‑3059. by facility‑based physicians who are not in your health plan. You may be responsible for payment of all or part of the fees for those Out‑of‑Network Visit: https://www.cms.gov/nosurprises/consumers for more information about Services, in addition to applicable amounts due for co‑payments, coinsurance, your rights under federal law. deductibles and non‑Covered Services. Speci昀椀c information about In‑Network and Out‑of‑Network facility‑based Newborns’ and Mothers’ Health Protection Act physicians can be found at www.MyHealthToolkitLA.com/links/FMOLHS and by Statement of Rights under the Newborns’ and Mothers’ Health Protection Act calling Member Services at (833) 468‑3594. You may access these websites from home. If you have any questions about how to do this, please contact Group health plans generally may not, under Federal law, restrict bene昀椀ts for any [email protected] or call 1‑833‑482‑7547. hospital length of stay in connection with childbirth for the mother or newborn child to less than 48 hours following a vaginal delivery, or less than 96 hours following a cesarean section. However, Federal law generally does not prohibit Certain services at an in-network hospital or ambulatory surgical center the mother’s or newborn’s attending provider, after consulting with the mother, When you get services from an in‑network hospital or ambulatory surgical from discharging the mother or her newborn earlier than 48 hours (or 96 hours center, certain providers there may be out‑of‑network. In these cases, the as applicable). In any case, plans and issuers may not, under Federal law, require most those providers may bill you is your plan’s in‑network cost‑sharing that a provider obtain authorization from the plan or the issuer for prescribing a amount. This applies to emergency medicine, anesthesia, pathology, radiology, length of stay not in excess of 48 hours (or 96 hours.) laboratory, neonatology, assistant surgeon, hospitalist, or intensivist services. These providers can’t balance bill you and may not ask you to give up your protections not to be balance billed. If you get other services at these in‑network facilities, out‑of‑network providers can’t balance bill you, unless you give written consent and give up your protections. You’re never required to give up your protections from balance billing. You also aren’t required to get care out‑of‑network. You can choose a provider or facility in your plan’s network. 60
CHIPs_ENGLISH_efc_7-31-22 Document Created 09/16/16 Page 1 of 2 Modi昀椀ed August 3, 2022 5:21 PM Premium Assistance Under Medicaid and the Children’s Health Insurance Program (CHIP) If you or your children are eligible for Medicaid or CHIP and you’re eligible for FLORIDA – Medicaid health coverage from your employer, your state may have a premium assistance program that can help pay for coverage, using funds from their Medicaid or CHIP WEBSITE https://www.昀氀medicaidtplrecovery.com/昀氀medicaidtplrecovery.com/hipp/ programs. If you or your children aren’t eligible for Medicaid or CHIP, you won’t index.html be eligible for these premium assistance programs but you may be able to buy PHONE 1-877-357-3268 individual insurance coverage through the Health Insurance Marketplace. For GEORGIA – Medicaid more information, visit www.healthcare.gov. A HIPP https://medicaid.georgia.gov/health-insurance-premium-payment- If you or your dependents are already enrolled in Medicaid or CHIP and you live WEBSITE program-hipp in a State listed below, contact your State Medicaid or CHIP of昀椀ce to 昀椀nd out if PHONE 678-564-1162, Press 1 premium assistance is available. GA CHIPRA https://medicaid.georgia.gov/programs/third-party-liability/childrens- WEBSITE health-insurance-program-reauthorization-act-2009-chipra If you or your dependents are NOT currently enrolled in Medicaid or CHIP, and PHONE 678-564-1162, Press 2 you think you or any of your dependents might be eligible for either of these INDIANA – Medicaid programs, contact your State Medicaid or CHIP of昀椀ce or dial 1-877-KIDS NOW or www.insurekidsnow.gov to 昀椀nd out how to apply. If you qualify, ask Healthy Indiana Plan for low-income adults 19-64 your state if it has a program that might help you pay the premiums for WEBSITE http://www.in.gov/fssa/hip/ an employer-sponsored plan. PHONE 1-877-438-4479 If you or your dependents are eligible for premium assistance under Medicaid All other Medicaid or CHIP, as well as eligible under your employer plan, your employer must allow WEBSITE https://www.in.gov/medicaid/ you to enroll in your employer plan if you aren’t already enrolled. This is called PHONE 1-800-457-4584 a “special enrollment” opportunity, and you must request coverage within IOWA – Medicaid and CHIP (Hawki) 60 days of being determined eligible for premium assistance. If you have MEDICAID https://dhs.iowa.gov/ime/members questions about enrolling in your employer plan, contact the Department of WEBSITE Labor at www.askebsa.dol.gov or call 1-866-444-EBSA (3272). MEDICAID 1-800-338-8366 PHONE HAWKI http://dhs.iowa.gov/Hawki If you live in one of the following states, you may be eligible for WEBSITE assistance paying your employer health plan premiums. The following HAWKI 1-800-257-8563 list of states is current as of July 31, 2022. Contact your State for more PHONE information on eligibility – HIPP WEBSITE https://dhs.iowa.gov/ime/members/medicaid-a-to-z/hipp HIPP PHONE 1-888-346-9562 ALABAMA – Medicaid KANSAS – Medicaid WEBSITE http://myalhipp.com/ WEBSITE https://www.kancare.ks.gov/ PHONE 1-855-692-5447 PHONE 1-800-792-4884 ALASKA – Medicaid KENTUCKY – Medicaid The AK Health Insurance Premium Payment Program Kentucky Integrated Health Insurance Premium Payment (KI-HIPP) Program WEBSITE http://myakhipp.com/ WEBSITE https://chfs.ky.gov/agencies/dms/member/Pages/kihipp.aspx PHONE 1-866-251-4861 PHONE 1-855-459-6328 EMAIL [email protected] EMAIL [email protected] MEDICAID https://health.alaska.gov/dpa/Pages/default.aspx KCHIP WEBSITE https://kidshealth.ky.gov/Pages/index.aspx ELIGIBILITY KCHIP 1-877-524-4718 ARKANSAS – Medicaid PHONE WEBSITE http://myarhipp.com/ KENTUCKY https://chfs.ky.gov MEDICAID PHONE 1-855-MyARHIPP (855-692-7447) WEBSITE CALIFORNIA – Medicaid LOUISIANA – Medicaid Health Insurance Premium Payment (HIPP) Program WEBSITE www.medicaid.la.gov or www.ldh.la.gov/lahipp WEBSITE http://dhcs.ca.gov/hipp PHONE 1-888-342-6207 (Medicaid hotline) or 1-855-618-5488 (LaHIPP) PHONE 916-445-8322 / (fax) 916-440-5676 MAINE – Medicaid EMAIL: [email protected] ENROLLMENT WEBSITE https://www.maine.gov/dhhs/o昀椀/applications-forms COLORADO – Health First Colorado (Colorado’s Medicaid PHONE 1-800-442-6003 TTY: Maine relay 711 Program) & Child Health Plan Plus (CHP+) WEBSITE Private Health Insurance Premium WEBSITE Health First Colorado Website: https://www.maine.gov/dhhs/o昀椀/applications-forms https://www.health昀椀rstcolorado.com/ PHONE 1-800-977-6740 TTY: Maine relay 711 PHONE Health First Colorado Member Contact Center: 1-800-221-3943 / State Relay 711 MASSACHUSETTS – Medicaid and CHIP CHP+ WEBSITE https://www.colorado.gov/paci昀椀c/hcpf/child-health-plan-plus WEBSITE https://www.mass.gov/masshealth/pa CHP+ PHONE Customer Service: 1-800-359-1991 / State Relay 711 PHONE 1-800-862-4840 TTY: 617-886-8102 WEBSITE Health Insurance Buy-In Program (HIBI): https://www.colorado.gov/paci昀椀c/hcpf/health-insurance-buy-program 1 of 2 PHONE HIBI Customer Service: 1-855-692-6442 61
CHIPs_ENGLISH_efc_7-31-22 Document Created 09/16/16 Page 2 of 2 Modi昀椀ed August 3, 2022 5:21 PM MINNESOTA – Medicaid TEXAS – Medicaid WEBSITE https://mn.gov/dhs/people-we-serve/children-and-families/health-care/ WEBSITE http://gethipptexas.com/ health-care-programs/programs-and-services/other-insurance.jsp PHONE 1-800-440-0493 PHONE 1-800-657-3739 UTAH – Medicaid and CHIP MISSOURI – Medicaid MEDICAID https://medicaid.utah.gov/ WEBSITE http://www.dss.mo.gov/mhd/participants/pages/hipp.htm WEBSITE PHONE 573-751-2005 CHIP WEBSITE http://health.utah.gov/chip MONTANA – Medicaid PHONE 1-877-543-7669 VERMONT– Medicaid WEBSITE http://dphhs.mt.gov/MontanaHealthcarePrograms/HIPP PHONE 1-800-694-3084 WEBSITE http://www.greenmountaincare.org/ EMAIL [email protected] PHONE 1-800-250-8427 NEBRASKA – Medicaid VIRGINIA – Medicaid and CHIP WEBSITE http://www.ACCESSNebraska.ne.gov https://www.coverva.org/en/famis-select WEBSITE https://www.coverva.org/en/hipp PHONE 1-855-632-7633 Lincoln: 402-473-7000 MEDICAID AND 1-800-432-5924 Omaha: 402-595-1178 CHIP PHONE NEVADA – Medicaid WASHINGTON – Medicaid WEBSITE https://www.hca.wa.gov/ MEDICAID http://dhcfp.nv.gov PHONE 1-800-562-3022 WEBSITE MEDICAID 1-800-992-0900 WEST VIRGINIA – Medicaid and CHIP PHONE NEW HAMPSHIRE – Medicaid WEBSITE http://dhhr.wv.gov/bms http://mywvhipp.com WEBSITE https://www.dhhs.nh.gov/programs-services/medicaid/health- MEDICAID 304-558-1700 insurance-premium-program PHONE PHONE 603-271-5218 CHIP 1-855-MyWVHIPP (1-855-699-8447) TOLL-FREE TOLL FREE FOR 1-800-852-3345, ext 5218 HIPP PROGRAM WISCONSIN – Medicaid and CHIP NEW JERSEY – Medicaid and CHIP WEBSITE https://www.dhs.wisconsin.gov/badgercareplus/p-10095.htm MEDICAID http://www.state.nj.us/humanservices/dmahs/clients/medicaid/ PHONE 1-800-362-3002 WEBSITE WYOMING – Medicaid MEDICAID 609-631-2392 PHONE WEBSITE https://health.wyo.gov/healthcare昀椀n/medicaid/programs-and-eligibility/ CHIP WEBSITE http://www.njfamilycare.org/index.html PHONE 1-800-251-1269 CHIP PHONE 1-800-701-0710 NEW YORK – Medicaid To see if any other states have added a premium assistance program since July 31, WEBSITE https://www.health.ny.gov/health_care/medicaid/ 2022, or for more information on special enrollment rights, contact either: PHONE 1-800-541-2831 U.S. Department of Labor U.S. Department of Health NORTH CAROLINA – Medicaid Employee Bene昀椀ts and Human Services WEBSITE https://medicaid.ncdhhs.gov/ Security Administration Centers for Medicare www.dol.gov/agencies/ebsa & Medicaid Services PHONE 919-855-4100 1-866-444-EBSA (3272) www.cms.hhs.gov NORTH DAKOTA – Medicaid 1-877-267-2323, Menu Option 4, WEBSITE http://www.nd.gov/dhs/services/medicalserv/medicaid/ Ext. 61565 PHONE 1-844-854-4825 Paperwork Reduction Act Statement OKLAHOMA – Medicaid and CHIP According to the Paperwork Reduction Act of 1995 (Pub. L. 104-13) (PRA), no persons WEBSITE http://www.insureoklahoma.org are required to respond to a collection of information unless such collection displays a PHONE 1-888-365-3742 valid Of昀椀ce of Management and Budget (OMB) control number. The Department notes OREGON – Medicaid that a Federal agency cannot conduct or sponsor a collection of information unless it is WEBSITE http://healthcare.oregon.gov/Pages/index.aspx approved by OMB under the PRA, and displays a currently valid OMB control number, http://www.oregonhealthcare.gov/index-es.html and the public is not required to respond to a collection of information unless it displays PHONE 1-800-699-9075 a currently valid OMB control number. See 44 U.S.C. 3507. Also, notwithstanding any other provisions of law, no person shall be subject to penalty for failing to comply with a PENNSYLVANIA – Medicaid collection of information if the collection of information does not display a currently valid WEBSITE https://www.dhs.pa.gov/Services/Assistance/Pages/HIPP-Program.aspx OMB control number. See 44 U.S.C. 3512. PHONE 1-800-692-7462 The public reporting burden for this collection of information is estimated to average RHODE ISLAND – Medicaid and CHIP approximately seven minutes per respondent. Interested parties are encouraged to WEBSITE http://www.eohhs.ri.gov/ send comments regarding the burden estimate or any other aspect of this collection of PHONE 1-855-697-4347, or 401-462-0311 (Direct Rite Share Line) information, including suggestions for reducing this burden, to the U.S. Department of SOUTH CAROLINA – Medicaid Labor, Employee Bene昀椀ts Security Administration, Of昀椀ce of Policy and Research, Attention: PRA Clearance Of昀椀cer, 200 Constitution Avenue, N.W., Room N-5718, Washington, DC WEBSITE https://www.scdhhs.gov 20210 or email [email protected] and reference the OMB Control Number 1210-0137. PHONE 1-888-549-0820 SOUTH DAKOTA - Medicaid OMB Control Number 1210-0137 (expires 1/31/2023) WEBSITE http://dss.sd.gov 2 of 2 PHONE 1-888-828-0059 62
New Health Insurance Marketplace Coverage Form Approved Options and Your Health Coverage OMB No. 1210-0149 (expires 6-30-2023) PART A: General Information When key parts of the health care law take effect in 2014, there will be a new way to buy health insurance: the Health Insurance Marketplace. To assist you as you evaluate options for you and your family, this notice provides some basic information about the new Marketplace and employmentbased health coverage offered by your employer. What is the Health Insurance Marketplace? The Marketplace is designed to help you find health insurance that meets your needs and fits your budget. The Marketplace offers "one-stop shopping" to find and compare private health insurance options. You may also be eligible for a new kind of tax credit that lowers your monthly premium right away. Open enrollment for health insurance coverage through the Marketplace begins in October 2013 for coverage starting as early as January 1, 2014. Can I Save Money on my Health Insurance Premiums in the Marketplace? You may qualify to save money and lower your monthly premium, but only if your employer does not offer coverage, or offers coverage that doesn't meet certain standards. The savings on your premium that you're eligible for depends on your household income. Does Employer Health Coverage Affect Eligibility for Premium Savings through the Marketplace? Yes. If you have an offer of health coverage from your employer that meets certain standards, you will not be eligible for a tax credit through the Marketplace and may wish to enroll in your employer's health plan. However, you may be eligible for a tax credit that lowers your monthly premium, or a reduction in certain cost-sharing if your employer does not offer coverage to you at all or does not offer coverage that meets certain standards. If the cost of a plan from your employer that would cover you (and not any other members of your family) is more than 9.5% of your household income for the year, or if the coverage your employer provides does not meet the "minimum value" standard set by the Affordable Care Act, you may be eligible for a tax credit.1 Note: If you purchase a health plan through the Marketplace instead of accepting health coverage offered by your employer, then you may lose the employer contribution (if any) to the employer-offered coverage. Also, this employer contribution -as well as your employee contribution to employer-offered coverage- is often excluded from income for Federal and State income tax purposes. Your payments for coverage through the Marketplace are made on an after-tax basis. How Can I Get More Information? For more information about your coverage offered by your employer, please check your summary plan description or contact . The Marketplace can help you evaluate your coverage options, including your eligibility for coverage through the Marketplace and its cost. Please visit HealthCare.gov for more information, including an online application for health insurance coverage and contact information for a Health Insurance Marketplace in your area. 1 An employer-sponsored health plan meets the "minimum value standard" if the plan's share of the total allowed benefit costs covered by the plan is no less than 60 percent of such costs. 63
PART B: Information About Health Coverage Offered by Your Employer This section contains information about any health coverage offered by your employer. If you decide to complete an application for coverage in the Marketplace, you will be asked to provide this information. This information is numbered to correspond to the Marketplace application. 3. Employer name 4. Employer Identification Number (EIN) 5. Employer address 6. Employer phone number 7. City 8. State 9. ZIP code 10. Who can we contact about employee health coverage at this job? 11. Phone number (if different from above) 12. Email address Here is some basic information about health coverage offered by this employer: • As your employer, we offer a health plan to: All employees. Eligible employees are: Some employees. Eligible employees are: • With respect to dependents: We do offer coverage. Eligible dependents are: We do not offer coverage. If checked, this coverage meets the minimum value standard, and the cost of this coverage to you is intended to be affordable, based on employee wages. ** Even if your employer intends your coverage to be affordable, you may still be eligible for a premium discount through the Marketplace. The Marketplace will use your household income, along with other factors, to determine whether you may be eligible for a premium discount. If, for example, your wages vary from week to week (perhaps you are an hourly employee or you work on a commission basis), if you are newly employed mid-year, or if you have other income losses, you may still qualify for a premium discount. If you decide to shop for coverage in the Marketplace, HealthCare.gov will guide you through the process. Here's the employer information you'll enter when you visit HealthCare.gov to find out if you can get a tax credit to lower your monthly premiums. 64
The information below corresponds to the Marketplace Employer Coverage Tool. Completing this section is optional for employers, but will help ensure employees understand their coverage choices. 13. Is the employee currently eligible for coverage offered by this employer, or will the employee be eligible in the next 3 months? Yes (Continue) 13a. If the employee is not eligible today, including as a result of a waiting or probationary period, when is the employee eligible for coverage? (mm/dd/yyyy) (Continue) No (STOP and return this form to employee) 14. Does the employer offer a health plan that meets the minimum value standard*? Yes (Go to question 15) No (STOP and return form to employee) 15. For the lowest-cost plan that meets the minimum value standard* offered only to the employee (don't include family plans): If the employer has wellness programs, provide the premium that the employee would pay if he/ she received the maximum discount for any tobacco cessation programs, and didn't receive any other discounts based on wellness programs. a. How much would the employee have to pay in premiums for this plan? $ b. How often? Weekly Every 2 weeks Twice a month Monthly Quarterly Yearly If the plan year will end soon and you know that the health plans offered will change, go to question 16. If you don't know, STOP and return form to employee. 16. What change will the employer make for the new plan year? Employer won't offer health coverage Employer will start offering health coverage to employees or change the premium for the lowest-cost plan available only to the employee that meets the minimum value standard.* (Premium should reflect the discount for wellness programs. See question 15.) a. How much would the employee have to pay in premiums for this plan? $ b. How often? Weekly Every 2 weeks Twice a month Monthly Quarterly Yearly • An employer-sponsored health plan meets the "minimum value standard" if the plan's share of the total allowed benefit costs covered by the plan is no less than 60 percent of such costs (Section 36B(c)(2)(C)(ii) of the Internal Revenue Code of 1986) 65
Important Contacts Bene昀椀ts Information FSA/HSA Retirement Plans askHR PayFlex 403(b) and 457(b) Plans [email protected] www.pay昀氀ex.com Lincoln Financial Group 833-482-7547 844-PayFlex (729-3539) www.LincolnFinancial.com/FMOLHS 877-562-4738 Medical Plan Basic Life/AD&D Blue Cross Blue Shield Supplemental Life/AD&D EAP www.MyHealthToolkitLA.com/links/ Long Term Disability New Directions fmolhs Lincoln National www.ndbh.com 833-468-3594 Life Insurance Company 800-624-5544 Dental Plan www.LincolnFinancial.com/FMOLHS Financial Wellness App 855-818-2883 Delta Dental Payactiv www.deltadentalins.com Leave Administration www.payactiv.com 800-521-2651 Short Term Disability [email protected] FMOLHS Leave 877-937-6966 Prescription Drug Coverage Administration Team Express Scripts (ESI) [email protected] Education Assistance Program www.express-scripts.com 833-482-7547 Wiley Beyond 877-816-8717 855-206-4965 Voluntary Critical Illness https://wbp.wiley.com/fmolhs Health and Well-Being Voluntary Accident Program Lincoln Financial Group Healthy Lives 855-818-2883 www.ourhealthylives.org www.LincolnFinancial.com/FMOLHS 855-426-4325 When contacting LFG, your ID is your Vision Plan full SSN. UNUM Vision www.alwaysassist.com 866-679-3054 66

Before you finish the enrollment process, did you remember to… See page 9 for details » Get your questions answered? on how to access Oracle » Review your bene昀椀t options? Employee Self Service » Review and update your personal information, from work or home. dependents and bene昀椀ciaries in Oracle Employee Self Service? » Enroll in core bene昀椀ts – Health, Dental, Vision, Medical FSA – within 30 days of your new hire/new eligibility date? » Enroll/Review Voluntary Bene昀椀ts within 30 days of your new hire/new eligibility date? » Click SUBMIT when you have completed your enrollment in Oracle Employee Self Service? » Save a printed copy of your bene昀椀t elections? » Upload dependent veri昀椀cation documents in Oracle Employee Self Service under Me/Bene昀椀ts/My Documents within 30 days of your new hire/new eligibility date? » Designate a bene昀椀ciary for your life insurance coverages? » If your bene昀椀t elections are properly completed and saved, you will get con昀椀rmation message on the screen that states, "Your bene昀椀t elections were saved." If you do not receive a con昀椀rmation message, your elections were not properly completed and you must complete the election process again within 30 days of your new hire/new eligibility date. » Go to My Bene昀椀ts card to view and print a copy of your elections. You must have a copy for your 2023 bene昀椀t elections to report a problem with your enrollment. Help is a phone call or click away. Reach out using the method that works best for you: » Submit an Oracle Service Request by clicking on Help Desk/HR Service Requests.* » Email [email protected] » 833-4UaskHR (833-482-7547) * This is the fastest method for getting an answer to your question.
