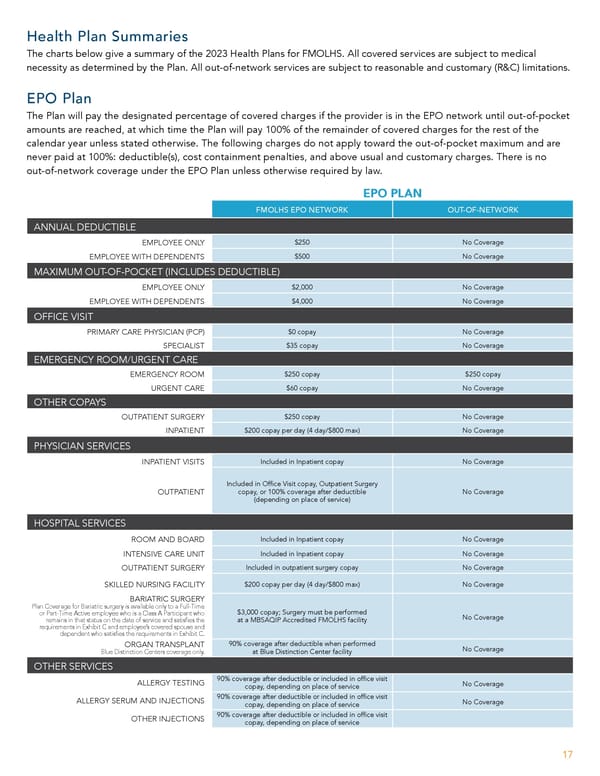
Health Plan Summaries The charts below give a summary of the 2023 Health Plans for FMOLHS. All covered services are subject to medical necessity as determined by the Plan. All out-of-network services are subject to reasonable and customary (R&C) limitations. EPO Plan The Plan will pay the designated percentage of covered charges if the provider is in the EPO network until out-of-pocket amounts are reached, at which time the Plan will pay 100% of the remainder of covered charges for the rest of the calendar year unless stated otherwise. The following charges do not apply toward the out-of-pocket maximum and are never paid at 100%: deductible(s), cost containment penalties, and above usual and customary charges. There is no out-of-network coverage under the EPO Plan unless otherwise required by law. EPO PLAN FMOLHS EPO NETWORK OUT-OF-NETWORK ANNUAL DEDUCTIBLE EMPLOYEE ONLY $250 No Coverage EMPLOYEE WITH DEPENDENTS $500 No Coverage MAXIMUM OUT-OF-POCKET (INCLUDES DEDUCTIBLE) EMPLOYEE ONLY $2,000 No Coverage EMPLOYEE WITH DEPENDENTS $4,000 No Coverage OFFICE VISIT PRIMARY CARE PHYSICIAN (PCP) $0 copay No Coverage SPECIALIST $35 copay No Coverage EMERGENCY ROOM/URGENT CARE EMERGENCY ROOM $250 copay $250 copay URGENT CARE $60 copay No Coverage OTHER COPAYS OUTPATIENT SURGERY $250 copay No Coverage INPATIENT $200 copay per day (4 day/$800 max) No Coverage PHYSICIAN SERVICES INPATIENT VISITS Included in Inpatient copay No Coverage Included in Of昀椀ce Visit copay, Outpatient Surgery OUTPATIENT copay, or 100% coverage after deductible No Coverage (depending on place of service) HOSPITAL SERVICES ROOM AND BOARD Included in Inpatient copay No Coverage INTENSIVE CARE UNIT Included in Inpatient copay No Coverage OUTPATIENT SURGERY Included in outpatient surgery copay No Coverage SKILLED NURSING FACILITY $200 copay per day (4 day/$800 max) No Coverage BARIATRIC SURGERY Plan Coverage for Bariatric surgery is available only to a Full-Time $3,000 copay; Surgery must be performed or Part-Time Active employee who is a Class A Participant who No Coverage remains in that status on the date of service and satis昀椀es the at a MBSAQIP Accredited FMOLHS facility requirements in Exhibit C and employee’s covered spouse and dependent who satis昀椀es the requirements in Exhibit C. ORGAN TRANSPLANT 90% coverage after deductible when performed No Coverage Blue Distinction Centers coverage only. at Blue Distinction Center facility OTHER SERVICES ALLERGY TESTING 90% coverage after deductible or included in of昀椀ce visit No Coverage copay, depending on place of service ALLERGY SERUM AND INJECTIONS 90% coverage after deductible or included in of昀椀ce visit No Coverage copay, depending on place of service OTHER INJECTIONS 90% coverage after deductible or included in of昀椀ce visit copay, depending on place of service 17
 Team Member Guide to Benefit Enrollment Page 16 Page 18
Team Member Guide to Benefit Enrollment Page 16 Page 18